Treatment of Manifestations
No formal management guidelines have been developed for NKH.
Current treatment is focused on:
For severe NKH, no treatment is effective in changing the natural history of developmental delays, spasticity, and intractable epilepsy. Specifically, glycine-lowering therapy is not effective in improving the affected individual's development, even when initiated at birth [Korman et al 2006]. However, glycine-lowering therapy does decrease the frequency and severity of seizures and is used as part of the overall epilepsy management of disease [Hennermann et al 2012]. It also improves attentiveness and resolves neonatal apnea.
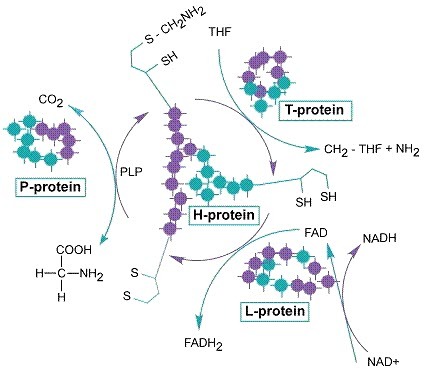
In contrast, for attenuated NKH current treatment consists of reduction of plasma concentration of glycine by treatment with sodium benzoate and blockade of NMDA receptors, which are overstimulated at the glycinergic site. To date two independent studies have shown that early, aggressive treatment of children with pathogenic variants associated with residual glycine cleavage enzyme system (GCS) activity who are likely to develop attenuated NKH resulted in improved neurodevelopmental outcome and reduced propensity for epilepsy [Korman et al 2004, Bjoraker et al 2016]. Further, in individuals with attenuated NKH, sodium benzoate improves alertness, reduces or eliminates episodic lethargy, and may also improve behavior.
Reduction of Plasma Concentration of Glycine
Sodium benzoate can reduce the plasma glycine concentration into the normal range (Table 1). The therapeutic goal is to lower the plasma glycine concentration into the low normal range, defined as 120 to 300 µmol/L for samples obtained one to two hours after a benzoate dose (timing is important).
The dose required depends on the glycine pool available. *
* Note: Because the glycine pool is reduced when individuals are on a ketogenic diet, sodium benzoate dose must be reduced upon initiation of this diet to avoid toxicity.
Sodium benzoate should be divided into no less than three doses per day; doses are more frequent in infancy (for example, neonates typically receive six daily doses).
Benzoate treatment begins with the lower dose range for the predicted disease severity; plasma glycine concentration is measured regularly. If the plasma glycine concentration is not within target range, the dose is increased by 50 mg/kg/day, and plasma glycine concentration is measured again as soon as 24 to 48 hours later. When glycine is within the target range, plasma glycine levels are measured regularly: every two weeks for infants, every month for young children, and every three months for older children.
Because the liver and kidney (but not the brain) are the sites of action of sodium benzoate, it is unclear to what extent administration of sodium benzoate reduces brain or CSF glycine. It is known that treatment with sodium benzoate does not normalize CSF glycine concentration. Follow up with serial measurements of CSF glycine concentration is not required.
Side effects of sodium benzoate include the following:
High-dose sodium benzoate (500-750 mg/kg/day) is frequently associated with gastritis, which may require oral administration of antacids, H2 antagonists, or proton pump inhibitors.
High-dose sodium benzoate in young infants can be associated with excessive loss of carnitine; those with low carnitine levels should receive supplementation to maintain normal plasma concentrations.
Dosing of sodium benzoate in excess of the individual requirement is dangerous: benzoate toxicity has high morbidity and mortality [
Van Hove et al 2005]. Hypocalcemia and low plasma glycine concentration (<150 µmol/L) can be early signs of sodium benzoate overdose. Measurement of plasma benzoate concentration can be helpful in evaluating potential toxicity (toxicity >2.5 mmol/L). Benzoate toxicity is treated by withholding benzoate, giving glycine, and/or hemodialysis.
As benzoate is unpalatable, a saliva-resistant granulated benzoate is available in several countries for individuals not on tube feeding. When transferring individuals from regular benzoate to granulated benzoate, providers should consider that the benzoate content in the granulated form is approximately 75%.
Glycine-restricted diet. In NKH, the contribution of dietary glycine is small compared to the excess in endogenous glycine synthesis versus endogenous catabolism of glycine. Infant formula is typically low in glycine; advancing the diet to intake of solid food introduces a small amount of extra dietary glycine. Restriction of dietary glycine can aid in controlling plasma glycine levels for some individuals with severe NKH. For many individuals a mild increase in the dose of sodium benzoate compensates for increased dietary intake of glycine.
An inappropriately severe glycine-restricted diet has been associated with protein malnutrition [Rogers et al 2014]; thus, the limited benefits of glycine restriction often do not outweigh the associated complexity and risk.
NMDA Receptor Site Antagonists
Glycine is an allosteric activator of the NMDA receptor channel complex; thus, excess glycine can result in overstimulation, which has been putatively linked to seizures and developmental delays. Clinically used partial inhibitors of the NMDA receptor include dextromethorphan, ketamine, or felbamate.
Dextromethorphan doses commonly range from 3 to 15 mg/kg/day, but individual variability is substantial. The authors have typically started at 10 mg/kg/day for neonates, 5 mg/kg/day for children, and 3 mg/kg/day for adolescents and adults, administered in three or four doses per day, or in twice-daily dosing if using a slow-release version (e.g., Delsym® Extended Release).
Pharmacogenomic differences exist in the metabolism of dextromethorphan, particularly based on CYP2D6 polymorphism. Some concomitant medications may slow the metabolism of dextromethorphan (e.g., cimetidine) and should be reviewed or not used as they may cause toxicity [Arnold et al 1997]. The effect of this in the treatment of NKH has not been reviewed. Blood concentration can technically be monitored; however, since the therapeutic level is not defined (should be >0 and <100 nmol/L), there is currently no clinically utility, and it is performed in a research context only [Hamosh et al 1998]. Overdose of dextromethorphan can cause increases in sleepiness and movement.
Treatment effect:
Attenuated NKH. Dextromethorphan used in combination with sodium benzoate has improved neurocognitive outcome and decreased seizure propensity. Improved attention, school performance, and behavior, as well as decreased chorea, have been observed in several individuals with attenuated NKH [Authors, personal observation]. In itself, high-dose dextromethorphan may have some anticonvulsant activity.
Severe NKH. The effect of dextromethorphan in severe NKH is dubious. Furthermore, the use of dextromethorphan in severe NKH is associated with a higher rate of pneumonia.
Oral ketamine has been used in NKH as an NMDA receptor antagonist. Improvement in outcome has been documented in attenuated NKH.
Glycinergic inhibitory receptors. Although strychnine improves tone and respiration, its use has been abandoned because of serious side effects that result from its long-term use.
Symptomatic Treatment
Seizure control. A systematic review of epileptic phenotypes, EEG patterns, and response to anti-seizure medications has rarely been done [Hennermann et al 2012].
Control of seizure disorders associated with a severely disturbed background such as burst suppression pattern or hypsarrhythmia is essential to allow developmental progress. Control tends to be challenging in severe NKH but is usually possible in attenuated NKH and essential for good outcome:
Severe NKH. Epilepsy propensity worsens in the first year of life, and from the second year of life, individuals have intractable epilepsy (i.e., daily seizures despite treatment with ≥2 anticonvulsants).
Attenuated NKH. First-line treatment is reduction of glycine levels with benzoate and dextromethorphan. This combination results in improvement of EEG background and reduced seizures; many individuals with attenuated NKH do not experience seizures on this treatment.
First-line treatment for newborns and infants with myoclonic seizures is benzodiazepines, with clobazam currently the preferred first-line drug, whereas older literature mentioned clonazepam and diazepam. Variable results are reported with use of standard anti-seizure medication (ASM) in neonates. Phenytoin has limited efficacy for seizure control. The effect of phenobarbital is variable in neonates, but because the nature of the epilepsy changes in late infancy, phenobarbital is often useful in treating seizures in older affected children.
Other drugs used with variable effect include levetiracetam and topiramate. Various ASMs have been used with variable success. Felbamate has been successful in some children with difficult-to-treat seizures. This treatment must be closely monitored for signs of liver or hematopoietic toxicity.
Ketogenic diet has been used in some individuals with variable success. Ketogenic diet always lowers the amount of glycine substantially and the dose of sodium benzoate should be reduced accordingly to avoid benzoate toxicity [Cusmai et al 2012]. Ketogenic diet has resulted in improved seizure control, but did not change hypsarrhythmic background.
For some older individuals with severe NKH and difficult-to-control seizures, a vagal nerve stimulator has been used with varying (sometimes very high) levels of success [Tsao 2010].
Treatment of infantile spasms and hypsarrhythmia in the context of severe NKH is difficult. Steroids rarely have an effect; vigabatrin has resulted in loss of skills and adverse outcome in individuals with attenuated NKH [Tekgul et al 2006; Authors, personal observation]. Glycine reduction with sodium benzoate, dextromethorphan, and other anticonvulsants has been the best approach for infantile spasms and hypsarrhythmia in attenuated NKH, whereas for severe NKH, treatment is difficult and conventional ASMs and ketogenic diet appear to have the best result – albeit often with only limited success.
Other. Gastrostomy tube placement should be considered early in the management of individuals with swallowing dysfunction associated with severe disease. Gastroesophageal reflux is common. Some individuals have benefited from a Nissen procedure. Chronic obstipation, a frequent problem in severe NKH, can be treated with laxatives.
Most affected individuals need physical therapy.
Scoliosis and hip dislocation, common in older children with severe NKH, are managed with standard techniques. The utility of these procedures has to be weighted in the quality of life of the individual.
Individuals with severe NKH have progressive difficulty maintaining good airway management. Pulmonary review and assistance can greatly facilitate quality of life.
Withdrawal of Intensive Care Support
Up to 80% of neonates with symptomatic NKH develop life-threatening bradypnea or apnea and require ventilator assistance during the first week of life. In the second to the third week of life spontaneous breathing typically resumes (even in the absence of treatment to reduce glycine levels), allowing discontinuation of ventilator assistance. Following resumption of spontaneous breathing, apnea is unlikely to recur. Following resolution of the apneic phase, some untreated infants with neonatal-onset NKH may die in the next two years, but many – if not most – live for several years.
Because of the generally poor prognosis of neonatal-onset NKH, some families elect to withdraw intensive care support during the neonatal apneic phase, allowing the infant to succumb prior to recovery of spontaneous respiration. For a discussion of the ethics involved in deciding to withdraw support for neonates with apnea see Boneh et al [2008].