One of the key goals of a health system is people-centredness: the ability to respond to both the medical and non-medical needs of the population (Papanicolas et al., 2022). In 2015, the WHO highlighted the critical role of people-centred healthcare in achieving UHC and significantly improving the health status of populations (WHO, 2015). In 2017, the OECD Health Ministerial Meeting further emphasized the importance of this theme. In response to the increasing focus on people-centred healthcare, the OECD developed the People-Centred Health Systems (PCHS) framework (OECD, 2021a). The framework defines a broad concept of people-centredness using measurable dimensions and domains that are key to making improvements that are relevant to people and their changing care needs. The OECD PCHS framework was published in 2021 and covers five dimensions for assessing the people-centredness of health systems: Voice, Choice, Co-production, Integration, and Respectfulness. These dimensions provide the methodological way to analyse the concept and serve as a strong starting point for assessing the people-centred agenda at the system level. That is, a people-centred approach is advocated for political, ethical, and instrumental reasons and is believed to benefit health service users, their families and carers, health professionals, and the health system in general (OECD, 2021a).
The COVID-19 crisis underscored the need for accountable, people-centred health services by highlighting weaknesses in public communication, disruptions in healthcare delivery, and severe restrictions on family visits. At the same time, the pandemic offered opportunities to improve people-centred care through real-time data sharing, increased public demand for involvement in policy-making, and the establishment of shared responsibility for addressing public health challenges (OECD, 2021c; Bollyky et al., 2022).
As elements of people-centredness are interwoven throughout the health system (Papanicolas et al., 2022), measuring it becomes a complex task, even with the framework at hand. People-centredness would start from the legal framework of the health system and possibilities for citizen participation in health policy-making (the dimension of Voice in the OECD PCHS framework) and stretch to ensuring the people-centredness at the level of service delivery (dimensions of Co-production and Respectfulness in the OECD PCHS framework) and beyond. Although the domains mentioned are not sufficient to describe the full scope of the people-centredness of the system, they are useful in addressing many practical policy issues that arise when defining people-centredness as a health system goal.
The first thorough exercise in collecting data for indicators on people-centredness was presented in the report Health for the People, by the People: Building People-centred Health Systems (OECD, 2021a), in the form of a scorecard that accompanied the framework. This work, together with that of Nolte, Merkur & Anell (2020), provides a solid basis for measuring people-centredness within the health system performance assessment based on concrete policy examples.
This section addresses the following policy questions:
- Does the system support the ability of health service users to act as the co-producers of care?
- Does the system enable people to participate in the development of health policy?
- Can improvements in people-centredness lead to increased trust in the health system?
Although trust is not an element of people-centredness, approaching this question through the prism of people-centredness explores the notion that the more people-centred health systems are, the more trust they can gain from the population.
Suggested indicators that could be used as tracers to explore the listed policy issues can help track potential improvements in system performance overall and across the HSPA frameworks.
4.1. Policy question: Does the system support the ability of health service users to act as the co-producers of care?
Moving away from the traditional healthcare professional-patient model, in which patients are passive receivers of care, is a crucial step in establishing a co-creative partnership. Achieving this requires policies that address the responsibilities of both parties. While many patient engagement strategies rightly emphasize the role of healthcare professionals in improving communication and fostering a collaborative relationship with their patients, it’s equally important for patients to take ownership of their role as co-creators of care (Batalden et al., 2016). For this to happen, healthcare providers should involve patients in discussions about their care and take sufficient time to provide that care (Nolte, Merkur & Anell, 2020). In addition, the information provided by doctors should be comprehensive and easy to understand, as patients need to have the health literacy and information necessary to make informed decisions (Moreira, 2018).
In general, by focusing more on people’s needs, people-centred care also encourages patients to co-produce health services, to be more involved in discussions about their treatment and to take more responsibility for their care (Nolte, Merkur & Anell, 2020). Professionals often underestimate patients’ ability to take responsibility for their health, although many patients are willing and eager to take on this responsibility if their abilities are recognized, supported, and encouraged, rather than ignored or undermined (Coulter & Oldham, 2016). Therefore, measuring aspects of co-production of health services can indicate the extent to which the health system is able to establish the delivery of people-centred services (Batalden et al., 2016).
Furthermore, healthcare that is equitable and promotes respect and dignity should be the norm, but is not necessarily the practice. A high level of personal attention and respectful and fair treatment are cornerstones of building a people-centred health system.
To address this policy issue, the use of some of the indicators proposed in the Co-production and Respectfulness dimensions of the OECD PCHS framework is helpful, and adds tangibility to an otherwise broad and philosophical concept of person-centredness overall and at the service delivery level.
While the people-centred components of service delivery can be numerous, the indicators below focus on those aspects of care that promote patient empowerment and co-creation. Performance indicators that help to assess people’s perceptions of the quality of services in terms of meeting their indirect needs include:
- Share of patients involved in decisions about their care
- Share of patients receiving easy-to-understand explanations
- Share of patients who spent enough time with their doctor
- Share of people agreeing that people are treated equally in their area
Share of patients involved in decisions about their care
The idea of a more participatory approach to informed decision-making was proposed as early as the 1970s. Shared decision-making gradually became the core of people-centred care. It is defined as an interpersonal, interdependent process in which health professionals, patients, and their carers relate to and influence one another as they work together to make decisions about a patient’s healthcare. Together, they consider the scientific evidence and the patient’s preferences and values before making a treatment choice (Légaré & Witteman, 2013).
There is evidence that patients generally want more information about their health and to play an active role in decisions about their care (Légaré et al., 2020). However, the underlying health problem, the treatment or care options and the actors involved, including the patients themselves, can influence the extent to which a decision can be shared. Healthcare providers report time constraints or attitudes – such as believing that patients want decisions made for them, or not being in the habit of involving their patients – as barriers to implementing shared decision-making in practice (Légaré & Witteman, 2013). There are also barriers on the patients’ side: the role patients want to play in the decision may depend on the nature of the health problem, their personal characteristics, or the level of trust between patient and healthcare professional.
Widespread implementation of shared decision-making in routine practice or at system level is not yet common. Given its crucial role in promoting people-centred health system performance, system-level evaluation is essential. Ongoing efforts include the identification of relevant theoretical models for measuring the impact and potential cost-effectiveness of shared decision-making. However, for a comprehensive assessment of this aspect as an indicator of people-centredness, nationally representative surveys, as suggested by Nolte, Merkur & Anell (2020), may be sufficient.
The Commonwealth Fund’s international survey, which includes questions on the practice of shared decision-making in healthcare, provides estimates for ten high-income countries. Fig. 4.1, based on the survey results, illustrates the experience of adults with chronic conditions in shared decision-making about the management of their condition or other health issues. On average, more than 35% of respondents said they hadn’t discussed their treatment goals or options with their healthcare professionals, which may indicate a need to update, re-evaluate, or strengthen quality standards that include shared decision-making as a foundation for service delivery.
Figure 4.1
Proportion of adults with a chronic condition who in the past year have not discussed their care goals or options with a health professional. Notes: SWE – Sweden, NOR – Norway, UK – United Kingdom, CAN – Canada, NET – (more...)
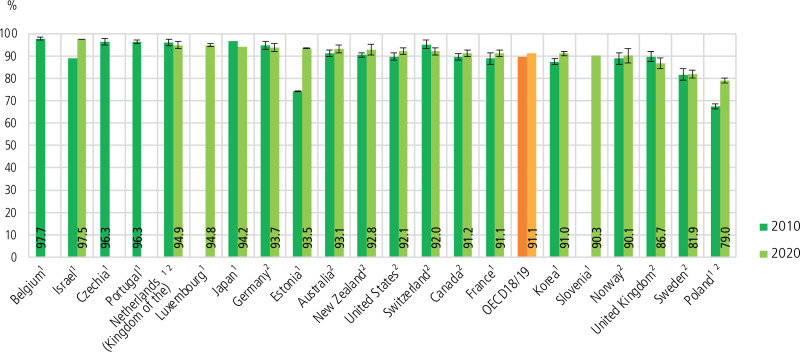
Figure 4.2
Share of patients reporting that they were given easy-to-understand explanations. Note: H lines show 95% confidence intervals. 1. Data from national sources. 2. Refers to patient experiences with regular doctor or regular practice. Source: OECD, 2021d, (more...)
This indicator is also included in the OECD Health Quality Indicators and is being proposed in the dimension of Co-production within the OECD PCHS framework. By the end of 2023, crude rates are available in the OECD database for a few countries, including Austria, Belgium, Estonia, Greece, Korea, Luxembourg, New Zealand, Portugal and Slovenia. Notably, only Estonia and Korea appear to collect these data on an annual basis. In 2024, the OECD will publish international patient-reported data for 18 countries, including the same indicator, as part of the Patient-Reported Indicator Surveys (PaRIS) (OECD, 2023).
Limitations and challenges of interpreting this indicator
As with any self-reported indicator, it may be affected by the patients’ own expectations or tendency to be more or less critical, together with the efforts of healthcare professionals. There are differences in preferences and readiness for shared decision-making, as well as different levels of literacy, and these individual differences can affect the results of surveys and assessments (Mira et al., 2014). In addition, internationally comparable results are highly dependent on comparable samples and the quality of the data collected. The indicator alone can give an indication of the capacity of health professionals to make shared decisions or the incentives in the system to do so, as determinants of people-centredness, but it doesn’t necessarily reflect the system of underlying policies and can be distorted by reporting bias.
Share of patients receiving easy-to-understand explanations
Another component of successful co-production and shared decision-making is receiving information that is sufficient and easy to understand. Communication barriers in healthcare can have a serious impact not only on the patient’s experience during the visit, but also on their overall health and safety. The whole healthcare system is based on the assumption that patients can understand complex written and spoken information, but communication within the healthcare system is not always organized in a way that enables, responds to, and encourages the participation of people with lower health literacy (Moreira, 2018). Therefore, if health professionals provide explanations that are understandable and appropriate for people with different levels of health literacy, this will not only lead to a gradual improvement in people’s health literacy, but also in their health outcomes (Epstein et al., 2005; Moreira, 2018; OECD, 2021c). Measuring whether people find doctors’ explanations easy to understand can indicate the system’s efforts to promote health literacy. However, the indicator routinely published by the OECD largely reflects the communication skills of health professionals and not the ability of the health system to provide appropriate health advice in different settings (including electronic health records, patient portals, etc.) and thereby promote the health literacy of the population at large. However, it is sufficient to assess people-centredness at the level of service delivery, as also proposed in the dimension of Co-production of the OECD PCHS framework (OECD, 2021a).
For example, in 2010, only 75% of Estonian citizens reported receiving comprehensible information during consultations. By 2020, this proportion had risen to 93.5%, reflecting the efforts to strengthen quality standards and introduce people-centred principles implemented in the 2008 National Health Plan, the main strategic document (Fig. 4.2).
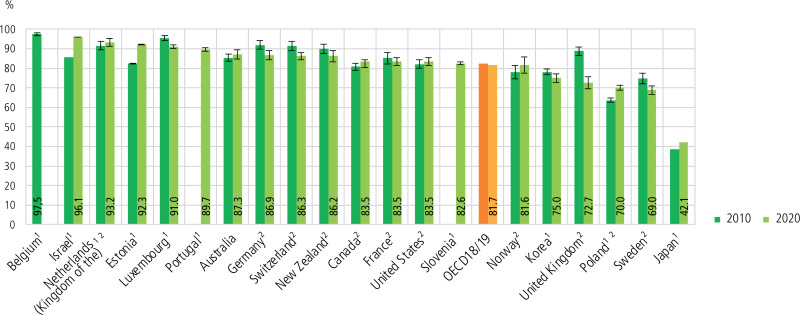
Figure 4.3
Doctor spending enough time with patient during consultation, 2010 and 2020 or latest available. Note: H lines show 95% confidence intervals. 1. Data from national sources. 2. Refers to patient experiences with regular doctor or regular practice. Source: (more...)
Limitations and challenges of interpreting this indicator
This aggregate indicator doesn’t take into account differences in patients’ health literacy. However, only such a patient-reported measure can help to assess the extent to which health professionals (for example, doctors) are able to meet these different literacy needs in practice (Epstein et al., 2005). Furthermore, the international comparison is hampered through lack of availability of data, as not all countries monitor this indicator as part of their routine quality monitoring.
Taken together, the proposed indicators of co-production help to measure the quality of service delivery in the area of people-centredness and it mainly reflects the interactions at the micro level of the patient-provider relationship. In addition, these measures assess the actual implementation of basic elements of people-centred care in clinical practice. Each indicator on its own can be traced back to specific arrangements made either at the level of resource generation or at the level of financing of services, but they all have the limitation of being subjective and prone to high scores from people with low expectations of their health service.
Share of patients who spent enough time with their doctor
Ensuring that the patient is heard, that the consultation is thorough, and that their care is tailored accordingly is fundamental to the delivery of people-centred care. This patient-reported measure tracks the extent to which patients feel the doctor spent enough time with them during the consultation. Time is an asset that enables shared decision-making, the identification of medical and non-medical needs, and the overall quality of healthcare. Data suggest that shorter consultations are detrimental to the care provided. There is evidence suggesting that longer consultations improve health promotion, patient empowerment, and quality of record keeping; they lead to more accurate diagnosis, improved quality of life, and patient empowerment. Many studies have also found that short consultation times are responsible for polypharmacy, overuse of antibiotics and poor communication with patients (Irving et al., 2017). Furthermore, sufficient consultation length not only demonstrates a people-centred focus on service delivery, but is also a quality indicator used by WHO and the International Network for the Rational Use of Drugs (INRUD) to promote safe and cost-effective use of medicines around the world.
Measuring such aspects of care, such as sufficient time for care, can guide policy-makers in reviewing the system of incentives that may encourage the provision of short but frequent consultations and thus, nominally, overuse of health services, or even in addressing the number of health professionals and the availability of resources (Nolte, Merkur & Anell, 2020).
Although there are different ways of measuring the average length of a consultation, for the purposes of assessing the people-centredness of a service and an individual’s experience, patient-reported measures are the best reflection of how much was enough for them and their needs at the time (OECD, 2021a). Across OECD countries, the majority of patients reported spending enough time with a doctor during the consultation, except for Japan, which could be associated with a high number of consultations per doctor (Fig. 4.3). However, it is precisely this type of in-depth investigation that is required to determine specific factors that may be influencing these changes.
Figure 4.4
People reporting that “All people are treated equally in GP services in my area”. Source: (Eurofound 2023)
Limitations and challenges of interpreting this indicator
There are many factors that contribute to international differences in patient-reported measures, including survey coverage, response rates, and cultural differences in response patterns. Furthermore, although the OECD recommends that data on patient experience in outpatient settings be collected through nationally representative population surveys, Japan and Portugal do so through service user surveys. In addition, about half of the countries presented collect data on patients’ experiences with a general practitioner, and the other half collect data on experiences with any outpatient physician. At the same time, the Commonwealth Fund’s International Health Policy Surveys 2010 and 2020 were used as a data source for 11 countries, although there are limitations in terms of small sample sizes and low response rates. Recently, new methods have emerged to address the limitations of patient-reported measures alone, and have begun to explore the idea of “concordance” of patient and clinician perspectives as an alternative in research of health system performance (Levesque et al., 2020).
Share of people agreeing that people are treated equally in their area
The impact of perceived discrimination by doctors is reflected in patient outcomes, as it has been associated with delaying or forgoing necessary medical care, including mental health services (Hausmann et al., 2011). Equal treatment or lack of discrimination on any grounds is a sign of people-centred care, which is also measured in international surveys (for example, the European Quality of Life Survey 2016). When asked “To what extent do you agree or disagree with the following statements about the GP, family doctor or health centre services in your area? All people are treated equally in these services in my area”, on average just over three-fifths of respondents in 22 countries answered in the affirmative, including almost half or less in Czechia, Greece, Italy and the Slovakia, and even less in Montenegro and Serbia (Fig. 4.4) (Eurofound, 2023). It is therefore important to collect patient-reported measures of perceived fairness and discrimination in healthcare, as they not only illustrate efforts to strengthen people-centredness, but also focus on improving the health of the population.
If a significant number of people perceive that the quality of care is not fair or equitable, this may indicate a number of systemic problems within the health sector. Such issues could include potential violations of human and patient rights, instances of discriminatory practices during treatment, whether experienced directly or indirectly; it could also be an indication of the overall robustness of the wider health system, reflecting aspects such as adequacy of funding and effectiveness of governance. This indicator can also reflect whether patients feel respected. Therefore, a low score on this indicator, when used to measure the people-centredness of healthcare, should prompt a more in-depth analysis and serve as a fundamental step in identifying relevant policy interventions, whether to improve the quality of service delivery, to strengthen the governance structures of the health system, or to address other relevant areas.
Limitations and challenges of interpreting this indicator
While this indicator may capture patients’ experience of service delivery, by design it is not strictly limited to this aspect. The current wording of the question (“To what extent do you agree or disagree with the following statements about the GP, family doctor or health centre services in your area? Everyone is treated equally in these services in my area”) may reflect people’s perceptions of the governance of the health system and their access to care. This is particularly true when considering media coverage of negative experiences of healthcare that others have had and reported.
It’s important to note that the indicator does not focus solely on discrimination, but the format of the question allows it to be included. Comparisons of survey data between countries should be made with caution, as cultural and personal biases may influence reporting. In addition, the indicator doesn’t distinguish whether perceived discrimination is based on personal experience or on individuals’ perceptions of others’ experiences.
How do these indicators help to monitor and transform support for service users to act as co-producers of care?
The discussed indicators serve as valuable tools for monitoring progress towards more people- (patient-) centred healthcare and have the potential to highlight disparities within the system. Despite weaknesses, together these indicators can lead to a deeper understanding of the reasons for the current level of co-production and respect in the delivery of health services. They allow us to assess the determinants of people-centredness, such as whether providers have the necessary skills for dignified communication and shared decision-making, whether they can serve patients with different levels of health literacy, and whether broader system improvements are needed. This could require adjusting appointment scheduling practices, payment models, improving the healthcare workforce, or introducing efficiency strategies to prevent hurried consultations and ensure comprehensive patient care. Additionally, these measures may provide input for policy development and the design of improved healthcare delivery models. If a significant number of patients feel that they are not included in decision-making, strategies could be introduced to require providers to involve patients in the planning of their care. Likewise, if patients experience difficulty in understanding the medical advice, offering additional patient education services or simplifying the language could prove useful.
Transforming a healthcare system to become more patient- and people-centred entails both structural changes and cultural shifts within the organization. It is essential to acknowledge and address the subjective nature of these indicators, interpreting them in light of the broader objectives and values of the health system.
4.2. Policy question: Does the system enable people to participate in the development of health policy?
People-centredness includes, but is not limited to, the extent to which citizens or patients are able to participate in healthcare decision-making, reflecting the overall governance of the health system and the area of population and civil society participation and others (Nolte, Merkur & Anell, 2020). The domain of governance and legal foundation for people-centredness is covered in the dimension Voice of the OECD PCHS framework (OECD, 2021a). The legal frameworks of some countries like Austria and Germany illustrate this. Here, the members of statutory health insurance funds can directly influence payer policy. Alternatively, in Luxembourg patient groups must be consulted in the development of disease-specific national plans. However, formal possibilities for participation in health policy-making don’t fully embody the people-centredness of the system (Hoon Chuah et al., 2018).
Thus, in this section we propose assessing the degree of possible participation in health policy by using following indicator:
- People having a formal role in health policy decision-making bodies or processes
People having a formal role in health policy decision-making bodies or processes
Strengthening the voice of patients and citizens in health system decision-making improves the people-centredness of the system, as health policies are designed with people’s needs in mind. However, not all countries involve patients in formal health policy processes. Such processes may include the design of benefits packages, the financing of health services, standards of care, or the planning, development, delivery, and evaluation of health services. A growing body of evidence suggests that increasing the role of patient voices in the development and delivery of health services can lead to services that are more relevant and responsive to users’ needs (Bombard et al., 2018). Furthermore, patient involvement in planning has been linked to the creation of novel and tailored services that better serve patients (Crawford et al., 2002).
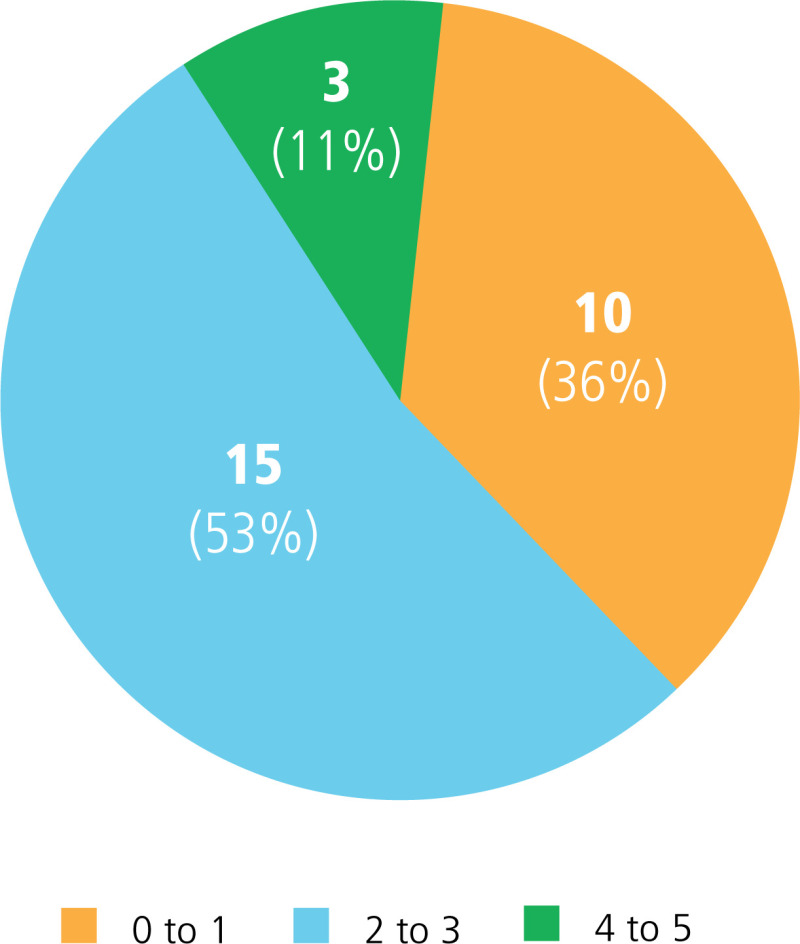
While the importance of a people-centred health system is widely recognized, the focus has primarily been on its application at the individual (patient) level. To build a health system that is centred on the people it serves, it is essential to recognize the critical role of involving individuals who use the health system, as well as their families and communities, in macro-level decision-making processes (Nolte, Merkur & Anell, 2020). A composite measure proposed by the OECD in the dimension Voice of its PCHS framework (OECD, 2021a) can be used for this purpose. The proposed score is based on countries’ responses to five questions that assess whether patients have a formal role in: 1) drug approval, 2) coverage or reimbursement, 3) health technology assessment, 4) service planning decisions, and 5) setting of public health goals. Fig. 4.5 shows the distribution of patient involvement in health policy-making across the 28 OECD countries that participated in the Health Systems Characteristics Survey. A higher number of areas that allow for citizen or patient participation doesn’t automatically mean a high level of people-centredness in practice, but it does show the historically higher priority and focus on multistakeholder participation in health policy-making.
Figure 4.5
Institutionalization of patients and citizens in decision-making. Note: Assesses whether patients have a formal role in: (1) licensing of pharmaceuticals, (2) coverage or reimbursement, (3) health technology assessment, (4) decisions related to service (more...)
Limitations and challenges of interpreting this indicator
Giving citizens and patients a role in formal processes recognizes the value of their insights and perspectives and helps to design responsive health systems. The lack of such representation in policy development can lead to a mismatch between the services provided and the real needs and expectations of the population. Thus, systems with limited opportunities for formal participation are, by design, less focused on people-centredness as the ultimate goal (OECD, 2021a).
Although giving citizens and patients a formal role in health policy-making is a sign of stronger people-centredness in the health system, the question is whether this role is large enough to influence the processes. Therefore, this indicator helps to assess the maturity of health system governance in terms of involving citizens in decision-making processes, but not the influence they can have.
How does this indicator help to monitor and transform people’s participation in the development of health policy?
Measuring formal opportunities for citizen participation in health policy-making helps in assessing the effectiveness of people-centredness at the ground level of governance and organization as a whole. By institutionalizing the voices of those whom the system serves, a sense of ownership and accountability is fostered within the community which has been involved in decision-making. Therefore, when this indicator shows active citizen participation across multiple domains, it signals a more adaptive system.
4.3. Policy question: Can improvements in people-centredness lead to increased trust in the health system?
People-centredness also includes how those who are not actively involved in healthcare feel about whether the system is meeting their needs. If people had a health need (medical or non-medical), would they trust and follow medical and health advice from the government or healthcare providers? When people trust health professionals, feel cared for, and have confidence in the health system’s ability to meet their needs, it promotes social cohesion and harmony, and achieves the goals of the health system (UNDP, 2020). Characteristics such as integrity, communication, confidence, and competence are often captured in measures of trust in healthcare. However, these are often limited to doctor-patient interactions and may not reflect the health system as a whole (Birkhäuer et al., 2017). As the COVID-19 pandemic demonstrated, the emergency response downplayed patients’ non-medical needs and used unclear communication strategies, undermining people’s trust in the health system’s ability to meet their needs and even contradicting key principles of people-centredness (Schloemer et al., 2021). This was compounded by pre-existing weaknesses and failures in the people-centredness of health systems, including the lack of overall quality of health services, accountability of governance structures and clear health communication strategies. This crisis of trust highlights the need to rebuild trust as an integral part of a resilient health system (Bollyky et al., 2022). Improving these areas of people-centredness can help to build trust in institutions and health systems and will be critical to meeting current and future health challenges.
The indicator that is used to describe a potential result of achieving higher people-centredness of the health system in this section is:
- Share of people who have trust in the health system
Share of people who have trust in the health system
Understanding and analysing trust requires recognizing two distinct but interrelated elements: 1) competence, or what concerns operational efficiency, or the ability, capacity, and good judgement to actually carry out a given mandate; and 2) values, or the underlying intentions and principles that guide actions and behaviours (OECD, 2021b).
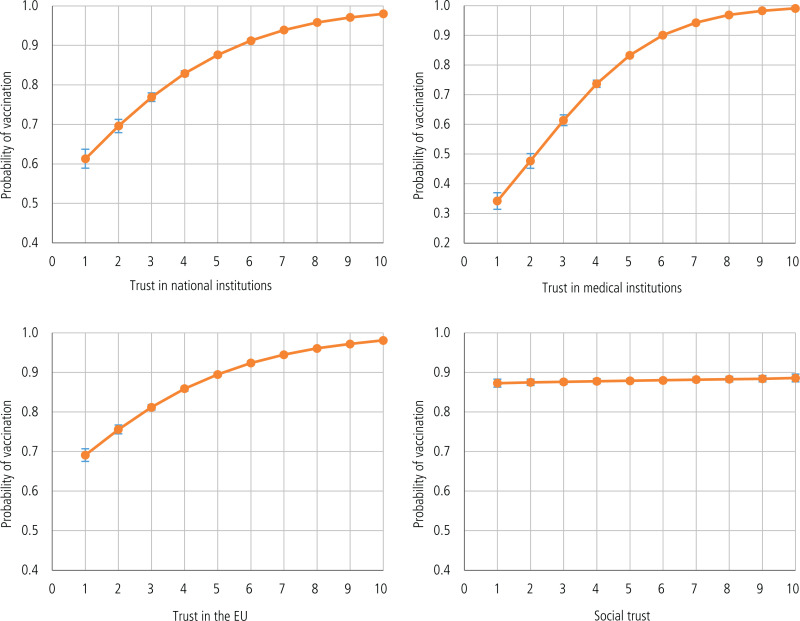
When healthcare is designed and delivered with a focus on patients’ needs, preferences, and experiences, it fosters trust and confidence in the system’s commitment to providing care that is people-centred (Ozawa & Sripad, 2013). The importance of measuring trust in health systems has increased in recent years, with the COVID-19 pandemic highlighting its critical importance. People with limited trust in the health ecosystem may engage in behaviours and attitudes that are detrimental to their health and well-being (Wesson, Lucey & Cooper, 2019; Beller et al., 2022). Furthermore, as seen in the COVID-19 example, perceptions of vaccine safety and agreement to follow other preventive measures were strongly influenced by the level of trust placed in the government (Eurofound, 2022). Fig. 4.6 shows that levels of trust in national, medical or EU institutions correlated with the likelihood of vaccination against COVID-19, whereas social trust appeared to have little or no effect.
Figure 4.6
Effect of trust in institutions on COVID-19 vaccine uptake. Source: Eurofound, 2022
Thus, people who trust institutions less were also less likely to follow official health advice on infection prevention. Of course, the COVID-19 crisis itself was an extraordinary situation that tested every aspect of life and governance. However, in “normal” circumstances, being aware of the level of trust people have in the health system and other stakeholders as a whole can help to promote a feedback loop to policy-makers. Policy-makers can then work to tailor health communication to different population groups or, more generally, to plan policies in a people-centred and participatory way from the outset.
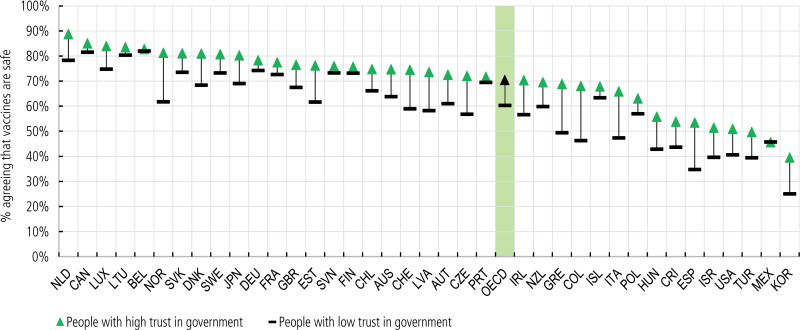
However, data from 28 OECD countries from before the COVID-19 pandemic show that the proportion of people who believe that “vaccines are safe” is higher among those with higher levels of trust in government than among those with lower levels of trust in government. This difference exceeds 15 percentage points in countries such as Canada, Denmark, Lithuania, Luxembourg, Netherlands (Kingdom of the), Norway, the Slovak Republic and Sweden (Fig. 4.7) (OECD, 2021b).
In general, the availability of data for international comparisons of trust in health systems can be hampered by fragmented national efforts and non-standardized methodologies for surveys on this topic. However, given the importance of this issue for improving the overall performance of health systems, initiatives are increasingly focusing on it. These range from more health market-focused research studies conducted as part of the Edelman Trust Barometer (Edelman Trust, 2022) to broader initiatives looking at how trust in health systems and governments can affect health behaviours (Wellcome Trust, 2020; Eurofound, 2022), and whether countries that generally have higher levels of uptake of official health advice for prevention could score higher in the area of people-centredness.
Figure 4.7
People with high trust are more likely to perceive vaccines as safe, although there are regional differences. Note: High trust is measured as “A lot” or “Some” trust in national government, and low trust measured as “Not (more...)
Limitations and challenges of interpreting this indicator
In light of recent public health threats, there is an urgent need to measure trust in the health system. This can serve as a barometer of public perceptions and guide efforts to rebuild trust, improve health system resilience, and promote a healthier, more informed and engaged population (Ozawa & Sripad, 2013). Furthermore, although measuring trust in the health system does not indicate the performance of the health system in the area of people-centredness at the macro level, yet it can open up the discussion about whether improving people-centredness would lead to achieving higher trust. This involves looking at different elements of interaction with the health system, including the quality of the patient-provider relationship, the effectiveness of communication and the accessibility of information at all levels, the extent to which people’s preferences are taken into account, and the overall quality and experience of care. Trust can also indicate the level of patient engagement in care, satisfaction, and the overall effectiveness of the health system (Gille, Smith & Mays, 2015).
Trust is a complex and multifaceted concept; measuring it through surveys reflects differences in personal experience, socioeconomic factors, and cultural or political nuances. However, individual perceptions of trust may make it difficult to compare even within the same cultural context, let alone across countries. The results of comparative surveys should be used with caution to avoid misleading conclusions.
Robust measures of trust can be used as indicators of health system performance, potentially highlighting the need for policy change, but there is no agreed methodology for measuring population trust in the health system. Ensuring the representativeness of the population surveyed and using standardized methodologies for data collection would be key considerations to address these limitations.
How does this indicator help to monitor and transform the role of people-centredness in increasing population trust in the health system?
By using trust as a measure, policy-makers can identify areas where system transparency and communication need to be strengthened to increase the reliability and responsiveness of the health system. The greater the level of trust, the more probable it is that individuals will partake in health-promoting behaviours, comply with medical advice, and contribute to a more cooperative public health environment. Overall, the indicators of formal participation and trust as a potential result of people-centredness can serve as benchmarks for potential growth. As such they are central to steering the continuing evolution of health systems towards greater transparency, inclusiveness, and trustworthiness.
4.3. Looking to the future
Several policy changes may contribute to improving the people-centredness of health systems, based on the tracer indicators outlined above. An important step would be to move from the traditional health professional-patient model to a co-productive partnership, with this new approach firmly embedded in the governance framework. This shift requires a comprehensive review of the responsibilities of all stakeholders, including a focus on empowering patients and promoting self-management. Healthcare providers must actively involve patients in discussions about their care and ensure that information is not only comprehensive but also easy to understand. This collaborative approach requires healthcare professionals, patients, and their carers to work together to make informed decisions about the patient’s healthcare. Overcoming barriers such as time constraints and differing attitudes to shared decision-making between healthcare professionals and patients is essential to achieving this goal. In addition, health professionals need to provide explanations that are tailored to people with different levels of health literacy. Policy-makers need to prioritize the strengthening of health literacy both in the population and in healthcare provision, promote the development of skills for co-creating healthcare in continuing medical education, and include these in quality standards, etc.
In addition to shared decision-making in healthcare, patients could play a more active role as co-creators and advisers in health policy and knowledge development, for example, in prioritizing research funding.
Policies aimed at strengthening the patient-provider relationship, improving communication, and ensuring access to information at all levels can better align health services with people’s preferences, thereby improving the quality of care and patient experience. This in turn can have a positive impact on patient engagement and satisfaction, and the overall effectiveness of the health system. Measuring trust in the health system is a valuable tool for understanding public perceptions and guiding efforts to rebuild trust, strengthen the resilience of the health system, and promote a healthier, more informed and engaged population.
Improving people-centredness requires measuring it. Although many promising initiatives are under way, health systems are generally data poor when it comes to patient-reported indicators. In the coming year, 2024, the OECD plans to publish the results of its first Patient-Reported Indicator Surveys (PaRIS)1, initiative, which will continue the ongoing efforts initiated by the OECD PHCS framework and focus on developing, refining, and improving further indicators of people-centredness and increasing their availability in the countries participating in this initiative (OECD, 2023). The continued and systematic adoption of this narrative by more countries promises improvements in the achievement of people-centredness as a goal of health systems.
References
- Batalden M, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25:509–17. Available at: https:
//qualitysafety .bmj.com/content/25/7/509 (accessed 7 December 2023) [PMC free article: PMC4941163] [PubMed: 26376674] - Beller J, Schäfers J, Haier J, Geyer S, Epping J. Trust in Healthcare during COVID-19 in Europe: Vulnerable groups trust the least. Z Gesundh Wiss. 2022:1–10. Available at: https://www
.ncbi.nlm .nih.gov/pmc/articles/PMC8944407/ (accessed 7 December 2023) [PMC free article: PMC8944407] [PubMed: 35345647] - Birkhäuer J, et al. Trust in the health care professional and healthoutcome: A meta-analysis. PLoS One. 2017;12(2):e0170988. [PMC free article: PMC5295692] [PubMed: 28170443]
- Bollyky TJ, Angelino O, Wigley S, Dieleman JL. Trust made the difference for democracies in COVID-19. Lancet. 2022;400(10353):657. [PMC free article: PMC9411258] [PubMed: 36030809]
- Bombard Y, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1):98. [PMC free article: PMC6060529] [PubMed: 30045735]
- Coulter A, Oldham J. Person-centred care: what is it and how do we get there? Future Hosp J. 2016;3(2):114–16. [PMC free article: PMC6465833] [PubMed: 31098200]
- Crawford MJ, et al. Systematic review of involving patients in the planning and development of health care. BMJ. 2002;325(7375):1263. [PMC free article: PMC136920] [PubMed: 12458240]
- Edelman Trust. Edelman Trust Barometer 2022. 2022. Available at: https://www
.edelman.com /trust/2022-trust-barometer (accessed 7 December 2023) - Epstein RM, et al. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med. 2005;61(7):1516–28. [PubMed: 16005784]
- Eurofound. Maintaining trust during the COVID-19 pandemic. Luxembourg: 2022. Available at: https://www
.eurofound .europa.eu/en/publications /2021/maintaining-trust-during-covid-19-pandemic (accessed 7 December 2023) - Eurofound. European Quality of Life Surveys (EQLS). Luxembourg: 2023. Available at: https://www
.eurofound .europa.eu/en/surveys /european-quality-life-surveys-eqls (accessed 7 December 2023) - Gille F, Smith S, Mays N. Why public trust in health care systems matters and deserves greater research attention. J Health Serv Res Policy. 2015;20(1):62–4. [PubMed: 25038059]
- Hausmann LR, Hannon MJ, Kresevic DM, Hanusa BH, Kwoh CK, Ibrahim SA. Impact of perceived discrimination in healthcare on patient-provider communication. Med Care. 2011;49(7):626–33. [PMC free article: PMC3117903] [PubMed: 21478769]
- Hoon Chuah FL, et al. Community participation in general health initiatives in high and upper-middle income countries: A systematic review exploring the nature of participation, use of theories, contextual drivers and power relations in community participation. Soc Sci Med. 2018;213:106–22. [PubMed: 30075416]
- Irving G, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7(10):e017902. [PMC free article: PMC5695512] [PubMed: 29118053]
- Légaré F, Witteman HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Aff (Millwood). 2013;32(2):276–84. [PubMed: 23381520]
- Légaré F, Härter M, Stiggelbout AM, Thomson R, Stacey D. Choosing treatments and the role of shared decision-making. In: Nolte E, Merkur S, Anell A, editors. Achieving person-centred health systems: evidence, strategies and challenges. Cambridge University Press; 2020. pp. 283–316.
- Levesque JF, Corscadden L, Dave A, Sutherland K. Assessing Performance in Health Care Using International Surveys: Are Patient and Clinician Perspectives Complementary or Substitutive. J Patient Exp. 2020;7(2):169–80. [PMC free article: PMC7427366] [PubMed: 32851137]
- Mira JJ, Guilabert M, Pérez-Jover V, Lorenzo S. Barriers for an effective communication around clinical decision making: an analysis of the gaps between doctors’ and patients’ point of view. Health Expect. 2014;17(6):826–39. [PMC free article: PMC5060922] [PubMed: 22897499]
- Moreira L. Health literacy for people-centred care: Where do OECD countries stand? OECD Health Working Papers No. 107. Paris: OECD Publishing; 2018. Available at: https://www
.oecd-ilibrary .org/social-issues-migration-health /health-literacy-for-people-centred-care_d8494d3a-en (accessed 7 December 2023) - Nolte E, Merkur S, Anell A. Achieving person-centred health systems: evidence, strategies and challenges. Cambridge University Press; 2020.
- OECD. Health for the People, by the People: Building People-centred Health Systems. OECD Health Policy Studies. Paris: OECD Publishing; 2021a. Available at: https://doi
.org/10.1787/c259e79a-en (accessed 7 December 2023) - OECD. An updated OECD framework on drivers of trust in public institutions to meet current and future challenges. OECD Working Papers on Public Governance No. 48. Paris: OECD Publishing; 2021b. Available at: https://www
.oecd-ilibrary .org/governance /an-updated-oecd-framework-on-drivers-of-trust-in-public-institutions-to-meet-current-and-future-challenges_b6c5478c-en (accessed 7 December 2023) - OECD. Strengthening the frontline: How primary health care helps health systems adapt during the COVID 19 pandemic. OECD Policy Responses to Coronavirus (COVID-19). Paris: OECD Publishing; 2021c. Available at: https://doi
.org/10.1787/9a5ae6da-en (accessed 7 December 2023) - OECD. Health at a Glance 2021: OECD Indicators. 2021d. https://www
.oecd-ilibrary .org/social-issues-migration-health /health-at-a-glance-2021_ae3016b9-en . - OECD. Patient-Reported Indicator Surveys (PaRIS). Paris: OECD Publishing; 2023. Available at: https://www
.oecd.org/health/paris/ (accessed 7 December 2023) - Osborn R, Squires D, Doty MM, Sarnak DO, Schneider EC. In new survey of eleven countries, US adults still struggle with access to and affordability of health care. Health Aff. 2016;35(12):2327–36. [PubMed: 27856648]
- Ozawa S, Sripad P. How do you measure trust in the health system? A systematic review of the literature. Soc Sci Med. 2013;91:10–14. Available at: https://www
.sciencedirect .com/science/article /pii/S0277953613002724 (accessed 7 December 2023) [PubMed: 23849233] - Papanicolas I, Rajan D, Karanikolos M, Soucat A, Figueras J. Health system performance assessment: a framework for policy analysis. Copenhagen: WHO Regional Office for Europe (on behalf of the European Observatory on Health Systems and Policies); 2022. Available at: https:
//eurohealthobservatory .who.int/publications /i/health-system-performance-assessment-a-framework-for-policy-analysis (accessed 7 December 2023) [PubMed: 37023239] - Schloemer T, Schröder-Bäck P, Cawthra J, Holland S. Measurements of public trust in the health system: mapping the evidence. Eur J Public Health. 2021;31(3):ckab165.360.
- UNDP. Strengthening social cohesion: Conceptual framing and programming implications. United Nations Development Programme; 2020. Available at: https://www
.socialcohesion .info/library/publication /strengthening-social-cohesion-conceptual-framing-and-programming-implications (accessed 7 December 2023) - Wellcome Trust. Wellcome Global Monitor 2020: Covid-19. 2020. Available at: https://wellcome
.org /reports/wellcome-global-monitor-covid-19/2020 (accessed 7 December 2023) - Wesson DE, Lucey CR, Cooper LA. Building Trust in Health Systems to Eliminate Health Disparities. JAMA. 2019;322(2):111–12. [PubMed: 31173060]
- WHO. Interim report. Geneva: World Health Organization; 2015. People-centred and integrated health services: an overview of the evidence. Available at: https://iris
.who.int /bitstream/handle/10665 /155004/WHO_HIS?sequence=1 (accessed 7 December 2023)
Footnotes
- 1
The PaRIS International Survey of People Living with Chronic Conditions is the first international survey of patient-reported health outcomes and experiences of adults living with one or more chronic conditions who are managed in primary or other ambulatory care settings. It is the first of its kind to assess the outcomes and experiences of patients managed in primary care across countries.
Publication Details
Copyright
Publisher
European Observatory on Health Systems and Policies, Copenhagen (Denmark)
NLM Citation
Karanikolos M, Adib K, Azzopardi Muscat Net al., authors; Figueras J, Karanikolos M, Guanais F, et al., editors. Assessing health system performance: Proof of concept for a HSPA dashboard of key indicators [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2023. (Policy Brief, No. 60.) 4, Assessing people-centredness.