NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Guideline Centre (UK). Emergency and acute medical care in over 16s: service delivery and organisation. London: National Institute for Health and Care Excellence (NICE); 2018 Mar. (NICE Guideline, No. 94.)
22. 7-day diagnostic radiology
22.1. Introduction
Diagnostic radiology plays a crucial role in the clinical assessment of patients with acute medical emergencies (AME); for example, a chest x-ray (CXR) can provide information in patients presenting with chest pain or shortness of breath that influences diagnosis and immediate management. More sophisticated radiological investigations such as computerised tomography (CT), magnetic resonance imaging (MRI), ultrasound (US) and ventilation perfusion (V/Q) scans can also provide important information in patients with AME across a spectrum of presenting complaints. There are certain specific conditions (for example, pulmonary embolism, acute stroke, subarachnoid haemorrhage, cauda equina syndrome or thoracic dissection) that require urgent radiology (for example, CT or MRI) to determine the need for certain critical interventions (for example, thrombolysis, blood pressure control or surgery).
While it would seem inconceivable that access to basic radiology (for example, CXR) could be anything other than universal in a hospital setting, it remains unclear whether such access to all diagnostic radiological services is clinically or cost effective. There is a strategic drive in the United Kingdom NHS to provide a seven day service with the aspiration of equality of access to high quality medical care throughout the week. The provision of a 7-day diagnostic service has been identified by NHS England as being crucial to all elements of patient care22 and the Royal College of Radiologists has produced standards for providing a 7-day service.30 There is also existing NICE guidance on specific conditions that would require a 7-day diagnostic service to be present (for example, diagnosis of stroke, head injury and deep vein thrombosis).
Currently there is variable access to diagnostic radiology both in terms of time of the day, day of the week and geographical location, with larger centres tending to provide better access. Whilst plain radiology (for example, a CXR) is, as stated above, universally available in all EDs at all times of the day and days of the week, access to more sophisticated radiology (for example, CT, MRI, US) varies enormously by time of day, day of week and even geographical location. Specifically, for example, some EDs will have access to CT scanning during the day but not at night, or to US scanning during the week but not at weekend; geographical networks may be in place to allow access to certain investigations in certain places which are not available at others.
Given this lack of consistency in access to diagnostic radiology, the guideline committee aimed to address the question “does the provision of seven day diagnostic radiology in hospital improve patient outcomes?” in order to help inform the configuration of seven day services in the NHS.
22.2. Review question: Does the provision of 7 day diagnostic radiology in hospital improve patient outcomes?
For full details see review protocol in Appendix A.
22.3. Clinical evidence
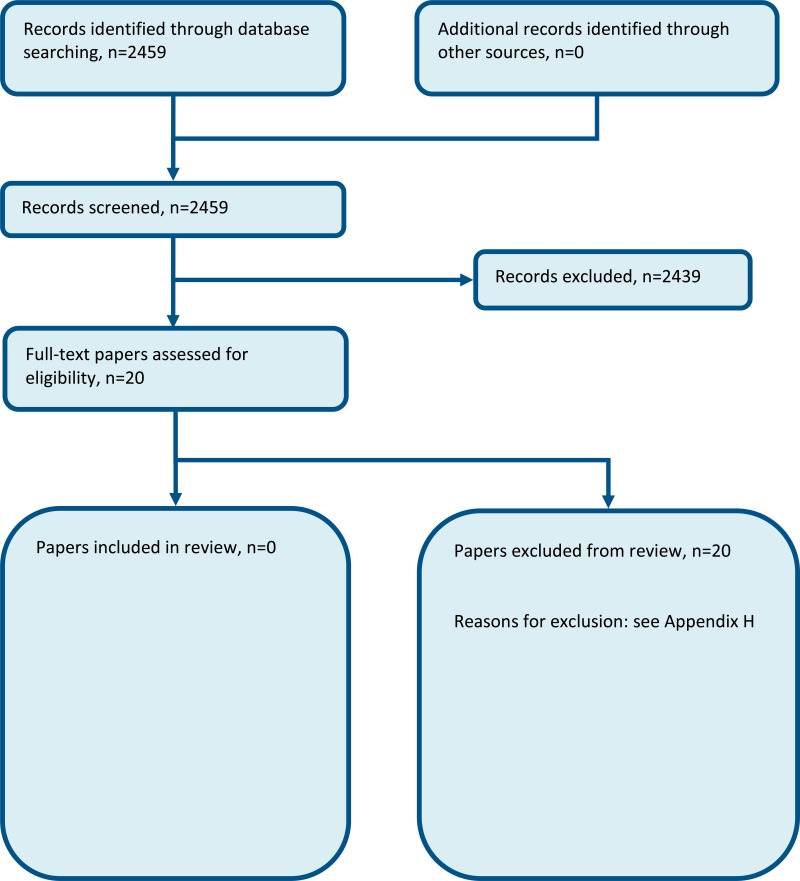
No relevant clinical studies comparing 24 hour access to diagnostic radiology with reduced access to diagnostic radiology were identified.
22.4. Economic evidence
Published literature
No relevant health economic studies were identified.
The economic article selection protocol and flow chart for the whole guideline can found in the guideline’s Appendix 41A and Appendix 41B.
In the absence of health economic evidence, unit costs were presented to the committee – see Chapter 41 Appendix I.
22.5. Evidence statements
Clinical
- No relevant clinical studies were identified.
Economic
- No relevant economic evaluations were identified.
22.6. Recommendations and link to evidence
| Recommendations | - |
| Research recommendations | RR12. What is the optimal configuration in terms of clinical and cost effectiveness of hospital diagnostic radiology services to support 7-day care of people presenting with medical emergencies? |
| Relative values of different outcomes |
Mortality, quality of life, length of stay, avoidable adverse events and patient and/or carer satisfaction were considered by the committee to be critical outcomes. Interval between request and receipt of result or report by the requesting healthcare professional, time to definitive diagnosis, staff satisfaction and representation were considered to be important outcomes. |
| Trade-off between benefits and harms |
The committee prioritised access to 7 day diagnostic CT, MRI, ultrasound and nuclear medicine. The committee identified plain film x-ray as an area where a 7-day service was routinely offered, and therefore they did not include this intervention within the evidence review as it would not change current practice. The provision of these services included 24/7, 7-day extended working, 7-day working (9am-5pm), 6-day working, and 5-day working. No evidence was identified for any combination of these. The committee considered the benefits of access to diagnostic radiology 7 days a week to be critical for many acute medical emergencies to ensure accurate diagnosis and timely and effective treatment. For example, immediate access to CT scans is essential for the investigation of suspected pulmonary embolism, intracranial haemorrhage and thoracic dissection. There are no anticipated harms in providing 7-day diagnostic radiology, if fully resourced. However, if shortages in radiology and radiography staff persist then there is potential for harm through spreading staff more thinly across the week or diverting them from other activities.. The committee discussed the lack of evidence identified and opted to develop a research recommendation. |
| Trade-off between net effects and costs |
No economic evidence was identified. Unit costs were presented to the committee (Chapter 41 Appendix I). No economic analysis could be conducted due to a lack of evidence on the benefits and harms. Increasing the provision and access to diagnostic radiology might require an increase in “up front” resources and therefore cost. This would include additional staff time and investment in radiology equipment and machinery where there is currently little provision. The current shortage of trained radiology and radiography staff means that the opportunity cost of expanding services is likely to be higher than that suggested by salary levels, since there is a need to recruit or train additional staff. Although the committee felt that it was likely to have a benefit and could potentially cause a decrease in length of stay, there was no evidence to show the cost impact or magnitude of benefit needed for the provision of a 7 day diagnostic service to be a cost-effective use of NHS resources. The committee decided that a recommendation could not be made due to a lack of evidence and therefore opted to form a research recommendation. |
| Quality of evidence | No evidence was identified. |
| Other considerations |
Currently there are varying levels of access to different types of radiology. The most common radiological investigations used for AME are plain film chest x-rays and CT scans. All hospitals should have 24/7 access to the former and most will have 24/7 access to the latter, both of which are critical for many AME scenarios. Access to more sophisticated types of radiology (for example, MRI scans or nuclear medicine) is currently much more limited, with larger centres more likely to provide these as a 7-day service. The committee noted that the provision of a 7-day diagnostic service has been identified by NHS England22 as being crucial to all elements of patient care and that the Royal College of Radiologists has produced standards for providing a 7-day service.30 Furthermore, there is existing NICE guidance on acute medical emergencies within specific medical conditions that would require a 7-day diagnostic service to be present. This includes guidance on:
The committee considered that immediate access to CT is also needed for other acute medical emergencies, such as thoracic dissection or pulmonary embolus. Rather than recommend research into the effectiveness of 7 day diagnostic radiology compared to no such provision the committee wished to target the research recommendation towards examining what a service supporting 7 day care would be comprised of. NHS radiology services have already made significant moves towards a 7 day service in recent times particularly in terms of diagnostic radiology provision. The committee noted that access to 7-day radiology encompassed access to the equipment as well as access to a person specialised in interpreting the result. They noted that there were some diagnostic radiological investigations for which consultants in non-radiological specialities were sufficiently skilled to provide an interpretation, for example, plain film chest x-rays, whilst MRI and CT would require special expertise. Remote (tele-interpretation) reporting would be possible and could be cost-effective, for example, interpretation from overseas during the night. There are case studies on the NHS England 7 day services website of centres providing 7 day imaging services for CT, MRI and ultrasound including some elective outpatient work at weekends. However, there would be occasions where direct interaction between clinician and radiologist would be needed and could provide added value. There is growing interest in computer-aided detection and diagnosis from radiological images. Were this approach to demonstrate an accuracy comparable to that of an expert radiologist, the potential impact on service delivery should also be evaluated. Interventional radiology is a more complex service to provide. The Royal College of Radiology (RCR)30 has provided guidance in the document produced by the Academy of Medical Royal Colleges on acute interventional radiology services. It is not possible, practical or affordable to offer such high-level services on all hospital sites. Networks or hub-and-spoke solutions may provide the services that are needed. Both require the movement of potentially acutely unwell patients. The interventional radiologist workforce would need to grow to provide this service throughout England. The Royal College of Radiology has already issued standards and guidance for delivering services:
The committee were aware that the provision of a 7-day radiological service may have a substantial cost implication. Therefore, they considered it to be important that any research into the components listed above be conducted with an analysis of cost-effectiveness. The committee were aware of reports from the National Imaging Clinical Advisory Group20 and Scottish Clinical Imaging Network27 on 7 day working in imaging that are available. |
References
- 1.
- Academy of Medical Royal Colleges. Seven day consultant present care: implementation considerations, 2013. Available from: http://www
.aomrc.org .uk/publications/reports-guidance /seven-day-implementation-considerations-1113/ - 2.
- Al Wattar BH, Frank M, Fage E, Gupta P. Use of ultrasound in emergency gynaecology. Journal of Obstetrics and Gynaecology. 2014; 34(2):172–173 [PubMed: 24456441]
- 3.
- Arnaoutakis GJ, Pirrucello J, Brooke BS, Reifsnyder T. Venous duplex scanning for suspected deep vein thrombosis: results before and after elimination of after-hours studies. Vascular and Endovascular Surgery. 2010; 44(5):329–333 [PubMed: 20484080]
- 4.
- Berner ES, Baker CS, Funkhouser E, Heudebert GR, Allison JJ, Fargason J et al. Do local opinion leaders augment hospital quality improvement efforts? A randomized trial to promote adherence to unstable angina guidelines. Medical Care. 2003; 41(3):420–431 [PubMed: 12618645]
- 5.
- Burton KR, Lawlor RL, Dhanoa D. The impact of a preauthorization policy on the after-hours utilization of emergency department computed tomography imaging. Academic Radiology. 2016; 23(5):588–591 [PubMed: 26947223]
- 6.
- Campbell JTP, Bray BD, Hoffman AM, Kavanagh SJ, Rudd AG, Tyrrell PJ et al. The effect of out of hours presentation with acute stroke on processes of care and outcomes: analysis of data from the Stroke Improvement National Audit Programme (SINAP). PloS One. 2014; 9(2):e87946 [PMC free article: PMC3922754] [PubMed: 24533063]
- 7.
- Carlos RC, Goeree R. Introduction: health technology assessment in diagnostic imaging. Journal of the American College of Radiology. 2009; 6(5):297–298 [PubMed: 19394569]
- 8.
- Chana P, Burns EM, Arora S, Darzi AW, Faiz OD. A systematic review of the impact of dedicated emergency surgical services on patient outcomes. Annals of Surgery. 2016; 263(1):20–27 [PubMed: 26840649]
- 9.
- Cubeddu RJ, Palacios IF, Blankenship JC, Horvath SA, Xu K, Kovacic JC et al. Outcome of patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention during on- versus off-hours (a Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction [HORIZONS-AMI] trial substudy). American Journal of Cardiology. 2013; 111(7):946–954 [PubMed: 23340031]
- 10.
- Ebinger M, Rozanski M, Waldschmidt C, Weber J, Wendt M, Winter B et al. PHANTOM-S: the prehospital acute neurological therapy and optimization of medical care in stroke patients - study. International Journal of Stroke. 2012; 7(4):348–353 [PubMed: 22300008]
- 11.
- Hardy M, Hutton J, Snaith B. Is a radiographer led immediate reporting service for emergency department referrals a cost effective initiative? Radiography. 2013; 19(1):23–27
- 12.
- Jamal K, Mandel L, Jamal L, Gilani S. ‘Out of hours’ adult CT head interpretation by senior emergency department staff following an intensive teaching session: a prospective blinded pilot study of 405 patients. Emergency Medicine Journal. 2014; 31(6):467–470 [PubMed: 23576233]
- 13.
- Khoo NC, Duffy M. ‘Out of hours’ non-contrast head CT scan interpretation by senior emergency department medical staff. EMA - Emergency Medicine Australasia. 2007; 19(2):122–128 [PubMed: 17448097]
- 14.
- Langan EM, Coffey CB, Taylor SM, Snyder BA, Sullivan TM, Cull DL et al. The impact of the development of a program to reduce urgent (off-hours) venous duplex ultrasound scan studies. Journal of Vascular Surgery. 2002; 36(1):132–136 [PubMed: 12096270]
- 15.
- Miller CD, Hoekstra JW, Lefebvre C, Blumstein H, Hamilton CA, Harper EN et al. Provider-directed imaging stress testing reduces health care expenditures in lower-risk chest pain patients presenting to the emergency department. Circulation Cardiovascular Imaging. 2012; 5(1):111–118 [PMC free article: PMC3272279] [PubMed: 22128195]
- 16.
- Moss JG, Murchison JT. Is radiology a ‘nine to five’ specialty? Clinical Radiology. 1992; 46(2):124–127 [PubMed: 1395400]
- 17.
- National Clinical Guideline Centre. Venous thromboembolic diseases: the management of venous thromboembolic diseases and the role of thrombophilia testing. NICE clinical guideline 144. London. National Clinical Guideline Centre, 2012. Available from: http://guidance
.nice.org.uk/CG144 - 18.
- National Clinical Guideline Centre. Head injury: triage, assessment, investigation and early management of head injury in infants, children and adults. NICE clinical guideline 176. London. National Clinical Guideline Centre, 2014. Available from: http://guidance
.nice.org.uk/CG176 - 19.
- National Collaborating Centre for Chronic Conditions. Stroke: diagnosis and initial management of acute stroke and transient ischaemic attack (TIA). NICE clinical guideline 68. London. Royal College of Physicians, 2008. Available from: http://guidance
.nice.org.uk/CG68 [PubMed: 21698846] - 20.
- National Imaging Clinical Advisory Group. Implementing 7 Day working inImaging Departments: Good Practice Guidance. Department of Health; 2012. Available from: https://www
.hislac.org /images/docs/policy-library /Implementing %207%20day%20working %20in%20imaging%20department.pdf - 21.
- Ng CS, Watson CJE, Palmer CR, See TC, Beharry NA, Housden BA et al. Evaluation of early abdominopelvic computed tomography in patients with acute abdominal pain of unknown cause: prospective randomised study. BMJ. 2002; 325(7377):1387–1389 [PMC free article: PMC138513] [PubMed: 12480851]
- 22.
- NHS England. NHS Services, Seven Days a Week Forum, 2013. Available from: https://www
.england.nhs .uk/wp-content/uploads /2013/12/forum-summary-report.pdf - 23.
- Notghi A, Mills AP, Harding LK. Out-of-hours weekend scintigraphy: assessing/predicting the need. Nuclear Medicine Communications. 1997; 18(9):857–860 [PubMed: 9352553]
- 24.
- Power ML, Cross SP, Roberts S, Tyrrell PJ. Evaluation of a service development to implement the top three process indicators for quality stroke care. Journal of Evaluation in Clinical Practice. 2007; 13(1):90–94 [PubMed: 17286729]
- 25.
- Raja FS, Amann J. After-hours radiology consultation in an academic setting, 2005-2009. Canadian Association of Radiologists Journal. 2012; 63(3):165–169 [PubMed: 21873025]
- 26.
- Redd V, Levin S, Toerper M, Creel A, Peterson S. Effects of fully accessible magnetic resonance imaging in the emergency department. Academic Emergency Medicine. 2015; 22(6):741–749 [PubMed: 25998846]
- 27.
- Scottish Clinical Imaging Network. Seven Day Working in Imaging in Scotland, 2015. Available from: http://www
.scin.scot .nhs.uk/wp-content/uploads /sites/3/2015/04 /2015-10-28-Recommendations-on-the-Implementation-of-Seven-Day-Working-in-Imaging-in-Scotland-V1 .pdf - 28.
- The Royal College of Radiologists. Standards for providing a 24-hour interventional radiology service. London: 2008. Available from: https://www
.rcr.ac.uk /sites/default/files /docs/radiology/pdf /Stand_24hr_IR_provision.pdf - 29.
- The Royal College of Radiologists. Standards for providing a 24-hour diagnostic radiology service. London: 2009. Available from: https://www
.rcr.ac.uk /sites/default/files /docs/radiology/pdf /BFCR(09)3_diagnostic24hr.pdf - 30.
- The Royal College of Radiologists. Standards for providing a seven-day acute care diagnostic radiology service. London. The Royal College of Radiologists, 2016. Available from: https://www
.rcr.ac.uk /sites/default/files /publication/bfcr1514_seven-day_acute .pdf
Appendices
Appendix A. Review protocol
Table 2Review protocol: Does the provision of 7 day diagnostic radiology in hospital improve patient outcomes?
| Review question | 7 day diagnostic radiology |
|---|---|
| Guideline condition and its definition | AME. Definition: people with suspected or confirmed acute medical emergencies. |
| Objectives | To determine if the increase access to investigations, diagnostics and interventions in ED & AMU improves outcomes. |
| Review population | Adults and young people (16 years and over) admitted to hospital with a suspected or confirmed AME. |
| Line of therapy not an inclusion criterion. | |
|
Interventions and comparators: generic/class; specific/drug (All interventions will be compared with each other, unless otherwise stated) |
24 hour access to diagnostic radiology. Reduced access to diagnostic radiology; 7-day extended working. Reduced access to diagnostic radiology; 7-day working (9am – 5pm). Reduced access to diagnostic radiology; 6-day working. Reduced access to diagnostic radiology; 5-day working. |
| Outcomes |
|
| Study design |
Systematic Review RCT Quasi-RCT Non-randomised comparative study Prospective cohort study Retrospective cohort study Case control study Controlled before and after study Before and after study Non randomised study |
| Unit of randomisation |
Patient. Ward. Hospital. |
| Crossover study | Permitted. |
| Minimum duration of study | Not defined. |
| Other exclusions |
Studies from non-OECD countries. Technological evaluation. Interventional radiology. Major trauma centres. |
| Population stratification |
CT. MRI. Ultrasound. Nuclear medicine. |
| Reasons for stratification | It is known that the stratified diagnostic radiology services have different utilisation and associated costs which will impact on the effectiveness of providing a 24-hour service. |
| Subgroup analyses if there is heterogeneity |
|
| Search criteria |
Databases: Medline, Embase, the Cochrane Library. Date limits for search: after 1990. Language: English only. |
Appendix B. Clinical study selection
Appendix C. Forest plots
No evidence to be included.
Appendix D. Clinical evidence tables
No evidence to be included.
Appendix E. Health economic evidence tables
No relevant health economic studies were identified.
Appendix F. GRADE tables
No evidence to be included.
Appendix G. Excluded clinical studies
Table 3Studies excluded from the clinical review
| Study | Exclusion reason |
|---|---|
| Al wattar 20142 | Inappropriate comparison. No comparator |
| Arnaoutakis 20103 | No outcomes of interest |
| Berner 20034 | Incorrect interventions. Presence of an ‘opinion leader’ |
| Burton 20165 | No relevant outcomes |
| Campbell 20146 | Incorrect interventions. Multivariate analysis with no analysis on radiology access |
| Carlos 20097 | Editorial |
| Chana 20168 | Systematic review |
| Cubeddu 20139 | Incorrect interventions. On-hours versus off-hours |
| Ebinger 201210 | Incorrect interventions. Access to mobile ambulance-based CT scanner |
| Hardy 201311 | Incorrect interventions. Immediate versus delayed reporting of radiology results |
| Jamal 201412 | Study design: diagnostic accuracy |
| Khoo 200713 | Study design: diagnostic accuracy |
| Langan 200214 | Inappropriate comparison. Comparison group had 24 hour radiology access |
| Miller 201215 | Technological evaluation |
| Moss 199216 | Study design: survey |
| Ng 200221 | Incorrect interventions. Early versus late CT scan |
| Notghi 199723 | Incorrect interventions. Retrospective theoretical intervention |
| Power 200724 | Incorrect interventions. Service reorganisation did not include change in radiology access |
| Raja 201225 | Inappropriate comparison. Comparison had 24 hour radiology access |
| Redd 201526 | Inappropriate comparison. Comparison had 24 hour radiology access |
Appendix H. Excluded health economic studies
No health economic studies were excluded.
Tables
Table 1PICO characteristics of review question
| Population | Adults and young people (16 years and over) with a suspected or confirmed AME in any part of hospital. |
|---|---|
| Intervention |
24 hour access to diagnostic radiology. Strata:
|
| Comparisons | Reduced access to diagnostic radiology as defined by:
|
| Outcomes |
|
| Exclusion |
|
| Study design | Systematic reviews (SRs) of RCTs, RCTs, observational studies only to be included if no relevant SRs or RCTs are identified. |