NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Center for Substance Abuse Treatment (US). Using Technology-Based Therapeutic Tools in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2015. (Treatment Improvement Protocol (TIP) Series, No. 60.)
Using Technology-Based Therapeutic Tools in Behavioral Health Services.
Show detailsIntroduction
In this chapter, you will meet several counselors who provide technology-assisted care (TAC) to clients who have mental or substance use disorders in various settings, including a student counseling center in a community college; an inpatient co-occurring disorders (CODs) unit in a large city; an Assertive Community Treatment (ACT) team at a community mental health center's (CMHC's) day hospital program; a pretreatment group in a rural area; a community behavioral health agency in a small city; and a CMHC that serves several counties. Each vignette begins by describing the setting, learning objectives, strategies and techniques, and counselor skills and attitudes specific to that vignette. Then a description of the client's situation and current symptoms is given. Each vignette provides counselor-client dialog to facilitate learning, along with:
- Master clinician notes: comments from the point of view of an experienced clinician about the strategies used, possible alternative techniques, and insights into what the client or prospective client may be thinking.
- How-to boxes: step-by-step information on how to implement a specific intervention.
The master clinician represents the combined experience of the contributors to this Treatment Improvement Protocol (TIP). Master clinician notes assist behavioral health counselors at all levels: beginners, those with some experience, and veteran practitioners. Before using the described techniques, it is your responsibility to determine if you have sufficient training in the skills required to use the techniques and to ensure that you are practicing within the legal and ethical bounds of your training, certifications, and licenses. It is always helpful to obtain clinical supervision in developing or enhancing clinical skills. For additional information on clinical supervision, see TIP 52, Clinical Supervision and the Professional Development of the Substance Abuse Counselor (Center for Substance Abuse Treatment, 2009b). As you are reading, try to imagine yourself throughout the course of each vignette in the role of the counselor. This chapter presents five vignettes, which can be briefly summarized as follows.
Vignette 1: Implementing a Web-Based Prevention, Outreach, and Early Intervention Program for Young Adults. This vignette discusses administrative issues in developing and implementing a Web-based prevention and intervention program and then demonstrates the capability of such a program to meet the stress management needs of a college student.
Vignette 2: Using Computerized Check-In and Monitoring in an Extended Recovery Program. This vignette demonstrates how computerized check-in and monitoring can support recovery for clients with co-occurring substance use disorders and serious mental illness (SMI).
Vignette 3: Conducting a Telephone- and Videoconference-Based Pretreatment Group for Clients With Substance Use Disorders. This vignette demonstrates how to serve clients in a rural area who are on a wait list for treatment by providing a pretreatment group conducted using video and telephone conferencing.
Vignette 4: Incorporating TAC Into Behavioral Health Services for Clients Who Are Hearing Impaired. This vignette describes ways in which TAC can support intake, assessment, referral, treatment, and continuing care for clients who are hearing impaired, a specific group of people for whom technology plays a particularly important role in access to care. Deaf clients and others in the Deaf community may prefer the term “Deaf” over “hearing impaired,” and you should adjust the terminology you use accordingly.
Vignette 5: Using Smartphones To Support Recovery for Clients With CODs. This vignette illustrates how mobile phone applications (apps) can be used to help clients with mental illness regulate their emotional responses, enhance the therapeutic alliance (between the client and counselor), and engage in effective coping strategies.
Vignette 1. Implementing a Web-Based Prevention, Outreach, and Early Intervention Program for Young Adults
Overview
This vignette introduces a prevention, outreach, and early intervention program that young adults can access via portable devices, such as smartphones and tablets, as well as via desktop computers. The program delivers intervention content through engaging technologies, including audio, video, text, and other interactive tools. It offers personalized assessments for alcohol, drug, and tobacco use; sexual health and sexually transmitted disease (STD) prevention; stress; nutrition; and other issues young adults may face. The program also offers psychoeducation, goal setting, action planning, cognitive–behavioral therapy (CBT), and skill-building tools. Programs like this one are packaged primarily for colleges and universities, but they can be customized to meet the needs of any population. This vignette first discusses some of the administrative issues in developing and implementing a Web-based prevention and intervention program; the second part of the vignette demonstrates the capability of such a program to meet the stress management needs of a college student. It then shows how the program might supplement early intervention efforts with an individual who is receiving counseling for a substance use disorder.
Learning Objectives
- Understand how to incorporate online screening tools into a larger program of prevention, screening, and early intervention for behavioral health difficulties.
- Identify individuals who need assistance and support by using an online screening tool for stress management.
- Use computer-assisted technologies to supplement ongoing counseling efforts and to extend traditional treatment services by providing support, education, and specific interventions.
- Become aware of issues that can arise when applying a technologically enriched, broad-based prevention and early intervention program with a specific target population.
- Evaluate the cost effectiveness of prevention and early intervention programs that include computer-assisted technologies.
Setting
John is a counselor in a local behavioral health center; his responsibilities include coordinating mental health and substance use disorder outreach and treatment services for students at the local community college. John and his two colleagues are seeing a significant increase in the number of stress-related requests for services from the student population. His center's resources are limited, so John has begun investigating online, client-driven tools that can be used with college-aged students in hopes of integrating such tools into his center's services. Students can access these resources from their computers or mobile devices. He hopes to be able to identify and appropriately serve three groups of people who may use behavioral health services: those with situational stress reactions, those who are experiencing significant stress and are at risk of more serious problems, and those who need acute care for pressing mental and/or substance use disorders.
In Part 1 of John's story, he searches for appropriate tools and meets with his program director to explore program development and implementation issues. In Part 2, John meets with Amy, a student experiencing significant stress, and helps her use the stress management component of the program to be able to continue in school and manage her school work. In Part 3, a student uses the program as an adjunct to counseling and mutual-help programs to address his drinking problem.
John's Story
Part 1. Providing targeted services
John, a senior counselor and college outreach coordinator for a local behavioral health center, is meeting with his program director, Nancy, to discuss how to provide better and more targeted services to students at the local college.
JOHN: I'm pulling my hair out with all these students coming in. I don't know why they're coming now. Maybe it's because it's the end of the semester, or maybe students have only just now begun to understand how they can benefit from help. We've just had an onslaught—more than we can really handle.
NANCY: What are the numbers?
JOHN: As you know, just three of us are handling this community college contract, and we've had 10 to 12 new students a week. They're coming in for stress-related issues and substance use. Alcohol problems are on the rise, and we're also seeing a lot more students smoking marijuana. Some of these kids are really under a huge amount of stress, but then again, I don't think others really need intensive services.
NANCY: So what are you thinking would be the best way to handle this increase?
JOHN: Well, I've done a little research, and I found some online resources that look pretty good. One is a comprehensive package for stress management, alcohol and drug use, nutrition, sexual health, and a variety of other topics. In this particular program, the students can go to the program Web site on their own, using a desktop computer, a laptop, a tablet, or even a smartphone. The site does some neat stuff based on education and CBT. There are a lot of cool tools that mirror things we already do clinically with students regarding prevention and relaxation. I wanted to talk with you about maybe integrating the package into our system of care.
NANCY: Do you know of any other college that's using this kind of program?
JOHN: Well, I don't have much spare time, you know? But I did some homework, and it seems like a number of colleges use this particular program. Some of them resemble our college, with an urban location, lots of commuting students, and limited treatment services for substance use and mental disorders. Some require all freshmen to do an orientation to the Web site, but others require that all students participate in just the alcohol and drug use part of the program. It looks like there are some data about the results and some evidence to support its use. I think it's pretty credible. What I like is that it's all contained in one package—just one stop and you'd have a range of resources to meet the variety of significant needs here in the college community.
NANCY: Can we get references from some of these other schools? I'd like to talk to them first. Also, I'm a little concerned about the all-inclusive package; it might be the case that not all elements of the package are high quality. We'll need to check into that.
JOHN: That's a good idea. I'll contact the colleges and talk to some of our colleagues there. I'll ask them about their experience with the program.
NANCY: I'd like to know whether there are other programs or other kinds of options. We could find out what the advantages or disadvantages are with them. I'd also be interested in how they measure success, and if we would measure it in the same way.
Master Clinician Note: Not everything that sounds good is good! Behavioral health service providers and program administrators must always ask questions and critically examine the evidence to determine whether a particular technology works or does what it purports to do. The National Registry of Evidence-Based Programs and Practices (NREPP) may have helped John and Nancy find some clarity as they struggled with these concerns. NREPP is supported by the Substance Abuse and Mental Health Services Administration (SAMHSA) and reviews programs and services that voluntarily seek such review. The NREPP Web site offers information and assistance related to identifying and assessing the evidence-based qualifications of any program (http://nrepp.samhsa.gov). John and Nancy could also decide to collect information about the results of whatever program they decide to use; doing so could help them determine how well the program is working with their population.
Other helpful Web sites include:
http://www.collegedrinkingprevention.gov/NIAAACollegeMaterials/Default.aspx
http://www2.edc.org/cchs/projects.html
http://www.dartblog.com/images/NH%20Alcohol%20Best%20Practices.pdf
JOHN: There are similar tools online that help kids handle stress better and improve their time management abilities, and some have risk reduction programs attached to their substance use packages.
NANCY: I think we'd be better off using what has been tested on other campuses with a similar group of people who have similar problems. Of course, there may also be some new, relatively untested programs that look good too.
JOHN: That makes sense.
NANCY: On the other hand, I know there is a lot of stuff out there already, some of it pretty well documented. I wonder if we can make up our own package, from scratch, to reduce costs.
Characteristics of Digital Comprehensive Assessment Tools
- Use of digital tools saves time and cost; it can also free up clinicians' schedules so that they can focus on other issues.
- Many comprehensive digital assessment tools are evidence based, provide reliable and concise information, and can address a broad range of issues relevant to specific populations, such as college students.
- Reporting features are available in some such tools; these features can assist clinicians in treatment planning.
- Digital assessment tools can reach people in need who are reluctant to access services through traditional delivery methods.
- Such tools can help provide ongoing client assessment.
- Some such tools are available to the consumer 24 hours a day, 7 days a week.
- Using digital assessment tools can provide continuity of care with automated message reminders about appointments, medication reminders, or preventive health facts.
Examples of Outreach, Screening, and Early Intervention Programs for College Students
- MyStudentBody (http://www.mystudentbody.com): This Web site contains a suite of online behavioral health interventions targeting risk issues central to young adults, including alcohol and drug use, tobacco use, HIV/STD prevention and sexual health promotion, stress, and nutrition. The interventions are grounded in motivational enhancement and evidence-based behavior change principles.
- eCHECKUP TO GO (http://www.echeckuptogo.com): This Web site provides online personal alcohol risk assessment and motivational feedback. In addition, psychoeducational and interactive tools build awareness of the consequences of alcohol use and support social norms.
- AlcoholEdu (http://www.everfi.com/alcoholedu-for-college): This online alcohol education program aims to reduce alcohol use and associated risks. It incorporates video, audio, and interactive tools to promote awareness about risky alcohol use and skills to avoid risky drinking.
- Drinker's Check-Up (http://www.drinkerscheckup.com): This Web site provides online alcohol risk assessments for individuals. There are three sections to the site: “Looking at your drinking,” “Getting feedback,” and “Deciding whether or not to change.” The instrument is brief and non-judgmental about alcohol use.
JOHN: Well, that's a choice we'll have to make. We could just find a couple of packages that address stress management and alcohol and drug use and not get into other issues, because there are packages that deal with these two issues specifically. The other option is to go in a more comprehensive direction, but the choices in that direction are more limited, at least right now.
The other thing that I think is important is deciding what level of stress, impairment, or pathology we're going to address. Do we want to take a broad approach, something to introduce all students to various problems and options? Do we want to screen for certain problems like stress, alcohol, and drugs? Do we want to offer options for people with significant situational stress? What about supplemental interventions for students with pretty serious alcohol and drug or mental health problems? Let's clarify our goals first and how we would measure our desired outcomes. That'll bring clarity in choosing a program.
Another issue is the evidence base for these programs. At least one is listed in NREPP (http://nrepp.samhsa.gov), and some of the smaller, less comprehensive packages probably have some research behind them, too. We also want to look at the evidence in the evidence-based program. Is it one small trial or more substantial research that supports the program? There's a lot to think about here.
NANCY: Yeah, there is. Did you find any data to suggest that any of these programs would either cost us more or save us money in the long run?
JOHN: Well, some of the programs definitely have costs involved. Some charge on a per-use basis, others seem to have a yearly subscription, and I would imagine there are some programs you can just buy outright. As for savings, if we can serve more students with the resources we have, then that cuts costs per unit of service. That would help us meet our goals more efficiently. Maybe we can do a pilot program for a year or so with some specific funding to try to understand the program's effectiveness, costs, and benefits.
NANCY: Don't you think this will increase the client flow, rather than reducing it?
JOHN: I'm hoping it'll reduce our workload and increase the client flow at the same time. We'll be screening more effectively by having students do a self-assessment. Students, before they decide to come in to see us in person, can take a computer-assisted self-assessment, learn a little about stress management, and then self-screen for substance use disorders and mental illness. Kids who are really in crisis and need immediate services will be able to bypass that and come right to us. It also lets us free up treatment time by providing online psychoeducational information at different stages in a client's change process.
It would also be more efficient in terms of our staff workload. If young people at lower risk receive education and a brief intervention online, we can spend more of our time on those kids who are struggling with more intransigent issues. The risk profile that the program creates after someone takes the personal risk assessment can be a really helpful reference if the individual does come to see us. It's a good place to start; it shows what he or she has been doing and offers strategies to reduce risks for that person.
NANCY: What about information technology (IT) support? Do we need any other system supports? We also need to think about liability and make sure we are covered there. What happens if the person is suicidal? We'll need a good response plan in place, and we have to make sure we monitor results to look for signs of danger.
JOHN: This particular resource that I looked at, and maybe others out there, actually runs on a server at the company that administers the program, and no software is installed on our system. We're not in charge of making it run. We'll need to make sure that the company we choose has a good tech support team and find out how they support clients. We'd also need to know how fast they respond to problems. The other schools that use these programs could give us a good idea.
NANCY: But I'm sure that counselors will have to provide some tech support to help students who need help accessing the program. We would also need to ensure that our clinical team is adequately trained and feels comfortable using the technology before we roll it out.
JOHN: If we were to recommend this program to students who come into the clinic, we would have to know, for instance, if they have enough bandwidth in their dorm room or at home to run it and access the videos and interactive activities on the Web site. I would also want to check with the IT staff at some other colleges to see if they have the capacity for students to use the program over the college wireless network. Of course, if students access the program on their own time with their own computers or mobile devices off campus, these issues may not be as significant. Regardless, we'll have the clients sign an informed consent form detailing their understanding of the benefits and potential hazards involved in working with us online.
NANCY: Does this program meet the capability requirements that the college recommends for student computer use? We should ensure that all students have access to the same service.
JOHN: I think it would be important to see if they could access it via their mobile devices, because most students have smartphones now. I think they can also access all of the program elements from a desktop or laptop.
NANCY: So what happens? They answer a bunch of questions about their stress and they get recommendations? What happens if they answer yes to all the questions, and they are at very high risk for suicide? How does it work then, when there is no actual person with them?
JOHN: Well, most programs don't assess specifically for suicide. It looks like most of them warn users who are experiencing acute stress or are having suicidal thoughts or behaviors to call an emergency number or hotline like the National Suicide Prevention Lifeline.
NANCY: Is there a message or a warning that says, “If you are experiencing extreme stress or other serious problems and you want to talk to a person live, here's what you should do?”
JOHN: What I really liked about this program is that when you subscribe, you can personalize the resources page to list the local resources in the community, at the community college, and at the health center. If someone is in crisis, they can call the emergency number here at the center.
There's another issue here that I don't want to overlook. Some kids from the college struggle with significant mental health and addiction crises—they're disabled with anxiety, have thought disorders, are depressed, or are drug dependent and scared to seek help. If this program can facilitate their entry into care, then we've provided a great service, and by intervening early, we may help them stabilize and begin recovery rather than getting worse before seeking treatment.
NANCY: You're probably right. Maybe some evaluative research after the program starts can help us track stabilization. How about the issue of confidentiality—we could potentially be collecting a lot of data on a broad spectrum of students. How do these programs control for that?
JOHN: In this particular program, data are stored on a secure server, not on an individual's computer or mobile phone. Each individual has a unique username and password they can use to access the program. There are algorithms behind the data so that individuals receive personalized feedback based on their response profile. There's also an administrative dashboard where administrators can see aggregate data as well as usage patterns.
Issues To Consider in Developing a Web-Based Outreach and Early Intervention Program
- Is the developer well known? Can the developer's references be checked? Does the developer have prior experience developing similar TAC programs? Is the program well supported by the developer?
- Are there empirical data to support that the program works? With which populations does it work? Are there published data? Does the program explicitly use evidence-based principles to guide behavior change?
- Are there a clear plan and resource list for users in significant distress or at high risk for self-harm?
- Is there assurance that all data entered into the system by participants are confidential and encrypted?
- Where will data be hosted, stored, backed up, and maintained?
- How will you obtain participant feedback about the program? How will you use that feedback in program development? Is the feedback aggregated or individual client data?
- Is there an administrative dashboard to monitor aggregate participant responses? Do these aggregate data reflect levels of impairment and actions taken by participants? Do the provided measures reflect the kinds of problems or questions participants have?
NANCY: So we would want to put something on the site about all of the 24-hour resources—hotlines and that sort of thing—that people can use in a crisis. It sounds interesting. Seems like there are a few more steps to take, but I think it's something that we should pursue.
JOHN: I agree. The program I'm thinking about tracks outcomes; we'd know how many students use it. We could ask students to evaluate it to see whether it's helping and what the limitations are. Maybe before we subscribe to the program, we could ask some students to get involved. That would take some of the burden off of us and help us test it to figure out what the best options are and whether they really meet the needs of the students.
After the meeting with Nancy, John researches the questions his administrator raised. He develops a plan that the university and the mental health center accept. They do live interviews with three companies that appear to meet their criteria, test each program, and check references. After analyzing their findings, they choose a program and begin a 1-year trial.
Part 2. Using screening tools to measure stress
This part of the vignette demonstrates how an online screening program can help students self-identify issues and situations in their lives that need attention.
As part of the program initiation, John is doing some trial demonstrations in classes on campus to gather data and establish a baseline stress level for students at his college. Next year, the program will be administered to all incoming freshmen, to at-risk students (students on academic probation, with disciplinary problems, or in violation of the college alcohol and drug use policy), and to any students who self-identify as needing counseling services. In conjunction with his audiovisual presentation, John describes a series of perceived stress situations and poses questions about alcohol and drug use in the past week to the students. He uses polling software to allow students to respond immediately to the questions, and then he reveals the aggregate classroom levels for each question in graphic form. John then invites students to assess where they stand in relation to the group average; some students are experiencing a good bit of stress, and some of these students may be drinking to cope with that stress at times.
He then tells the class that they can use the online program to learn more about stress and how to manage feeling overloaded without having to go to a therapist or counselor right away; he lets them know that they can take a personal assessment, get feedback, learn about stress and how it affects the body, and practice some healthy coping skills (e.g., exercise, meditation, deep breathing, music) to counteract those effects. John makes sure to tell them that, if after trying out the program, or even without reviewing the program, they want to seek professional help, they can visit his clinic or check the program Web site for contact information on other local resources.
After conducting one such classroom presentation, John stays to answer questions. Several students approach him, one of whom is Amy. She is concerned about some of her scores on the stress scale, which are higher than those of her peers. John makes an appointment for her to come to the mental health center so that they can talk in more detail.
JOHN: So Amy, how are you?
AMY: Sorta bad. I'm worried because my score on the stress test that you gave us in class yesterday was in the high range. I know I've been under a lot of pressure, but it worries me that my scores are so high. I really do think I'm having trouble concentrating. My grades aren't as good as they need to be to keep my scholarship, I'm having trouble sleeping, and the few friends I do have here tell me I'm being grouchy.
JOHN: Well, I'm glad you came in. Is there anything you're worried about?
AMY: I don't know if I'd call it worried. I'm from out of town. I'm here on full scholarship. I'm supposed to maintain a 3.0 grade point average, but last semester, I got a 2.8. So that's not good.
JOHN: Well, what happened?
AMY: The work is really hard, and I'm having trouble focusing. Maybe I just don't belong here.
JOHN: How do you think I could be helpful?
AMY: Fix me!
JOHN: What would that mean—to fix you?
AMY: If I lose my scholarship, I'm in trouble. I really need to get my grades up, so that's really stressing me. Then, on the other hand, because I'm so stressed, I have trouble sleeping, trouble motivating myself to study, trouble with almost everything. [She begins to tear up.]
JOHN: So, if I understand correctly, you need to find a way to bring your grades up, and that'll take off a lot of stress? Reducing the stress some will make it easier for you to get your grades up.
AMY: I guess so. I started feeling terrible; now I'm eating more, and I'm 10 pounds heavier than when I got here last fall. I spend so much time studying that I haven't made a lot of friends. Other people go out and have a good time, and I spend most of my time in my dorm room.
JOHN: Things are piling up.
AMY: I'm not sure that this school is the right place for me. But I also don't think I need counseling or therapy. By the time I get ready to come over here, then get back to the dorm, I've wasted at least a couple of hours that I could spend writing a paper or being in the library. I just need to get my grades up.
Advantages and Disadvantages of Using Web-Based Programs in Counseling
Advantages:
- Encourage self-assessment
- Reinforce stress management strategies/plans
- Foster provision of well-developed, clear action plans
- Open additional avenues for noncrisis support
Disadvantages:
- Lack the immediacy of in-person meetings
- Pose potential difficulties with understanding how to use the program
- Provide diagnostics without clear, scheduled follow-up and action plan
- Are contraindicated for work with suicidal, homicidal, or psychotic clients
In gauging the advantages and disadvantages of using Web-based counseling—or, indeed, any given technology in clinical practice—remember that, as always, use of good clinical judgment is imperative.
JOHN: I can understand your feeling that coming here just adds something else to your workload. But would you be willing to check something out? I have an idea about helping you get started on taking some action without having to come over here—something you can do on your own time, if you're willing to explore it.
AMY: Sure! It won't hurt.
JOHN: How are you with technology? Do you go online? Are you on Facebook?
AMY: Sure.
JOHN: Would you be willing to check out a Web site? It's the program I spoke about in class.
AMY: Well, I guess so.
JOHN: The first thing you'll do in the program is log in with a username and password that you devise, so that all of your information is confidential and accessible only to you. Once you're logged into the program, you'll then complete a personal profile that includes questions about your level of stress, the kinds of things that stress you out, and what you currently do to manage stress when you're feeling overloaded. It's a slightly longer version of the questionnaire you took in the classroom. You'll get feedback, tips, and information based on your profile. Then you'll have access to the information, interactive tools, and other activities in the program that you can review in whatever order you wish, whenever you wish. The tools and activities will help you identify triggers for what stresses you out, strengthen your coping skills for managing stress in healthy ways, and learn how to avoid stress, such as through time management strategies and getting good sleep. You can use these tools however you want, and you can add the ones that you find particularly helpful to a personal, interactive action plan that you can develop.
AMY: Can I use my phone to get into the program, or just my laptop?
JOHN: Do you have a smartphone?
AMY: Yeah.
JOHN: Then you can use your phone. Why don't I give you the link to the Web site? You can check it out right now.
AMY: You mean right now, like here in your office?
JOHN: Yes, let's be sure you can access the program. Then we'll take a minute to look over some of the content and see if you have any questions.
How To Encourage Clients To Use, and Continue Using, Web-Based Programs
- Give clear instructions about what to expect from the program and how to access the Web site.
- Demonstrate access and use of the program before the client leaves your office.
- Emphasize confidentiality and protection of private information (e.g., via passwords).
- Use a reminder system, such as text messaging, email, or an electronic calendar.
- Invite clients to report, in and out of the office, their successes and struggles with the program.
- Use secure video conferencing, encrypted email, or secure text messages to highlight client improvements and thereby promote motivation to continue using the program.
AMY: [Amy accesses the Web site on her cell phone.] This is pretty cool. There's a lot of stuff here.
JOHN: It's a comprehensive program to help people manage a variety of situations in their lives. I'm particularly interested in you looking into the stress management resources in the program. You can go on there and pick out the ones that you think will best meet your needs.
AMY: I don't know what that means.
JOHN: When you access the program, you'll answer some questions. Then you'll get feedback, just like you did in class earlier in the week. Based on your profile, it will highlight areas for you to check out on the site. I remember that you mentioned time management; this program has some tools to help you with that and also some other stress management techniques, like meditation and mindfulness.
AMY: I'm not really into that new-age stuff.
JOHN: Some people think of it as new-age stuff, but it might be something that you want to check out.
AMY: Is it like stretching?
JOHN: Something like that—stretching your mind.
AMY: That sounds interesting. How does that work?
JOHN: Well, it involves several steps. There are some assessment tools to help you evaluate how you use your time, and the program will give you information about ways to manage your time better. There are even some functions that actually help you make a plan for how you can use your time more effectively. Just go on the Web site and choose the time management and stress management tools you'd like to start with.
AMY: I'm not sure about this, but I'll check it out.
JOHN: Let's check back in a few days. Check out the program, and then we can talk about it.
AMY: But it was a hassle to come here. Is it okay for me to just send you an email or a text?
JOHN: Well, my reservation about that is that email isn't confidential. What if we do this: We have an encrypted email system here at the center, so I'll send you an email through that system right now. Then, when you reply to let me know how things are going in a week or so, that reply email will be encrypted. But be aware that anyone who might have access to your phone or your email will have access to our communication. Are you okay with that?
AMY: Well, not really. Maybe I should just give you a call.
JOHN: Okay, I'll look forward to your call in a few days. Do you have Skype or a similar video conferencing app on your computer?
AMY: Yeah. I use it with my parents every week and call friends back home with it.
JOHN: Great. Just call me, and we can videochat. My email is moc.chblacol@nhoj.
AMY: Okay. I like the idea of not having to come here every week. I'll just use the Web site in the next couple of weeks and check in by videochat to let you know how things are going.
JOHN: Sounds good. It was great to meet you, and I look forward to working with you.
AMY: Yeah. Me too.
During the next month, Amy uses the Web site on a number of occasions. She especially benefits from the time management, stress management, and sleep-related components of the program. She and John have two videochats during this month. She assures John that she will call if she begins to experience more distress than she is comfortable handling on her own.
Master Clinician Note: Counselors and administrators should be sure that clients fully understand how their agency's Web-based communications system works so that clients have realistic expectations about counselor availability, how long it may be before they receive responses to messages they send, and how the system is monitored. For example, will clients receive feedback? What are the client's expectations about feedback?
Part 3. Using Web-based interventions to support addiction recovery
Pete is referred to the student counseling center for violating the campus alcohol use policy; campus police found him sleeping in his car in the student parking lot, smelling strongly of alcohol and with an open six-pack of beer on the passenger-side floor of his vehicle. He was referred to the campus alcohol and drug policy office, where he was, in turn, referred to John's behavioral health center for an assessment. The following section of John's vignette details John's first meeting with Pete.
JOHN: Sounds like you have a lot going on, Pete. Do you have an idea of what you want right now?
PETE: I've tried to cut back on my drinking, and sometimes it works, but then I go back to it.
JOHN: What kinds of things have you tried?
PETE: Just willpower. I'll get drunk, then I'll feel terrible and miss class. My girlfriend threatened to break up with me because she said I got out of control one night. I just feel like I have to cut back, but I haven't been very successful doing that. Night before last, I drank a lot and then had to be at class yesterday morning. Between classes I went to the car, just to have a beer to take the edge off, and I guess I went to sleep. I must have been sleeping about 30 minutes when the cops rapped on the window and woke me up.
JOHN: Do you have some concerns about your drinking?
PETE: Yeah, but I've seen celebrity rehabilitation shows on reality TV, and I don't need that. I don't need to be sent away. I've tried Alcoholics Anonymous (AA), and there were some older folks in there who were fanatics. I don't want to be a fanatic about it. I just want to cut back on my drinking.
[John and Pete explore Pete's drinking history. Pete is cooperative in revealing a history of heavy drinking that began about 8 years ago and really became a problem while he was stationed at remote sites in the Air Force. Since his discharge 6 months ago, he has continued to drink daily. Upon returning to his hometown, he found that most of his old friends had moved on and weren't available. He started community college 3 months ago, but he hasn't really made friends. Mostly, he hangs out in his room at his parents' home or in a local pub, where he has met a few people. He has been dating a woman he met at the orientation session for the community college. He likes her a lot.]
JOHN: Well, let's talk for a few minutes about what you might want to do about your drinking. You say you aren't interested in treatment or in AA.
PETE: No! I don't want to go in front of a bunch of people and talk about my drinking.
[John continues to help Pete explore his options, including AA, other mutual-help programs, and inpatient and outpatient care, but Pete is adamant that he doesn't want community-based services. John assesses and does not find the need for detoxification or acute medical care. Pete must accept the recommendations of the counseling center as a condition of his staying in school, so John does have some clout, but at the same time, he wants Pete to feel ownership of his treatment plan. They settle on a three-pronged approach that includes an 8-week assessment group in which students with campus alcohol or drug infractions evaluate their substance use in a structured educational/discussion group setting at the college counseling center, completion of a Web-based alcohol and drug self-assessment that is part of the Web-based program adopted by the counseling center (along with a brief drug prevention education program that is part of the same package), and attendance at 10 online AA meetings.]
PETE: I have some reservations about this online AA thing. You say I don't have to give my name? All I have to do is go to the site and sign in?
JOHN: That is the beauty of it. You just go to this Web site. It operates similarly to other AA meetings and services. The Web site is http://www.aa-intergroup.org. All you need to do is sign in and then choose whether you want to attend an online meeting via videochat or telephone. The site also has chat rooms, email lists, and discussion forums. There are groups for specific populations, such as military personnel and veterans; people who are hearing impaired; gay, lesbian, bisexual, and transgendered people; and even groups for specific areas of the country. You have lots of choices. Some meetings are open and can be attended by anyone, regardless of whether they use alcohol or have a drinking problem; other meetings are closed to all but people who have a drinking problem and a desire to quit drinking.
Evidence-Based Alcohol and Drug Use Prevention Education Programs for College-Aged Populations
Evidence-based online alcohol and drug use prevention education programs for college-aged populations (e.g., MyStudentBody, AlcoholEdu, eCHECKUP TO GO) are grounded in motivational enhancement and social learning theories. Such programs typically include a self-assessment with personalized feedback to build motivation for behavior change and education about the risks of alcohol and drug use to promote accurate risk perceptions. The more comprehensive online programs (i.e., MyStudentBody, AlcoholEdu) also offer audio or video peer stories and interactive tools that foster coping skills for reducing alcohol and drug use and help individuals develop their own action plans for change. Most of the available online programs are subscription based, so that a participating college/university can subscribe for use by their entire student body or by targeted risk populations. For more information, visit:
PETE: Does that mean that I have to have a desire to quit drinking totally?
JOHN: Well, I think for your first few meetings, you can be undecided about whether you want to stop totally. Part of the agenda for the next couple of months—the assessment group, the online meetings, and the work on the Web site that we discussed you using—is to help you decide what you need to do.
PETE: I guess I'd be willing to try it. I can't guarantee that I'll want to quit drinking entirely, but I'd be willing to try the treatment plan we've laid out and see what it's like.
JOHN: That seems fair enough.
PETE: There is something I haven't told you—my girlfriend says that I have to do whatever you recommend, or she won't go out with me anymore. I really don't know how much I actually want to do all of this stuff, but I'm willing to do it to keep my girlfriend and to stay in school.
JOHN: So the stakes are high and it might be worth it to take the risk.
PETE: Yeah!
Pete completed all three sections of his treatment plan. He attended an online AA group, which offered a good introduction to how AA works and dispelled some myths Pete had subscribed to about what meetings would be like. No participants were from his area of the country, but in the assessment group, he did meet two other men who attend Young People in AA, an AA group for people ages 16 to 27. He has attended two meetings with them and says he got a lot from attending. His attendance at online AA helped him make the transition to local meetings. He has had no alcohol in 3 weeks now and came to the decision to stop drinking of his own accord. He completed the alcohol and drug use section of the Web-based program and used the summary report of his risk profile and feedback in his work with John. Pete appreciates the ongoing ability to access the program online to reassess his risks and review material to reinforce his action plan for sobriety. Pete also has a friend who was willing to go to AA but did not have a car, so Pete introduced him to online AA, thus expanding his friend's access to AA support and giving Pete the opportunity to experience how helping others can be part of his own recovery.
Online Recovery Support
Online recovery support communities (some specifically for young people), such as AA and Marijuana Anonymous, hold online meetings that allow participation through the telephone or through voice or text chat features on a computer or mobile phone. Reliable online recovery resources include:
Vignette 2. Using Computerized Check-In and Monitoring in an Extended Recovery Program
Overview
This vignette demonstrates how computerized check-in and monitoring can support recovery for clients with co-occurring substance use disorders and SMI. The vignette includes examples of how checking in via a desktop computer, tablet, or mobile phone can benefit both clients and staff members in managing recovery; how to build clients' engagement with the check-in process as part of their recovery plan; how to teach the basics of computer use to clients who are not already computer literate; how computerized check-in can more readily involve hard-to-engage clients in taking responsibility for their recovery; and how to help clients use technology to maintain a connection to treatment resources after formal treatment has been completed. These technologies can be useful in a variety of behavioral health settings to help clients maintain self-management, recognize potential relapse factors, and see long-term progress in recovery.
Learning Objectives
- Identify how a computerized check-in process can be used in behavioral health settings.
- Introduce skills for counselors in educating clients, particularly those who are not computer literate, to the use of computers for check-in and monitoring.
- Address problems that can arise when clients do not check in or are unable to complete the check-in process.
- Demonstrate how to use a computerized check-in process to monitor progress and changes over time for a client in recovery from CODs. The term “co-occurring disorders” indicates that a person has both a substance use disorder and a mental disorder and that neither disorder is caused by the other; both are independent disorders that warrant individual treatment.
- Engage clients in taking responsibility for their recovery process.
Setting
Sondro is completing short-term restabilization in an inpatient CODs unit in a large city. He has been hospitalized on multiple occasions. He typically does well in the hospital and for a short time after release. After that, however, he tends to disappear from treatment, not take prescribed medication, use drugs, and show signs of paranoid thinking, all of which cascades into Sondro ending up homeless, unable to take care of himself, physically ill, and at serious risk for psychological and physical trauma. The staff wants to provide continuity of care that may help Sondro stay on track in his recovery. If unit staff can help him identify early symptoms, intervention may be possible before he gets out of control.
Staff members identify two approaches in care that may help Sondro achieve these goals. First, they recommend a transition from inpatient care to an intensive outpatient day treatment setting. After completing the day program, he will receive intensive support and monitoring by the ACT team at the local CMHC. ACT services are specialized, intensive services that often go beyond the traditional delivery model of care, which can be limited to the client coming into a clinic and having little access to after-hours contact. Some ACTs offer availability 24 hours a day, 7 days a week, for some type of service; many include contacts with clients outside of the clinic setting.
Sondro's various service providers have agreed to a high level of treatment consistency and communication. One unifying element in Sondro's transition through these treatment environments is a computerized check-in process that Sondro will complete daily. The variables monitored by the check-in process are identified in the vignette. A significant benefit of the check-in process is the opportunity for Sondro to participate more actively in his own care and recovery.
Sondro's Story
Part 1. Developing client and counselor collaboration to support recovery
The treatment team wants to coordinate Sondro's care and transitions among the inpatient program, day treatment program, and ACT team services so as to provide ongoing care. Sondro will be attending the day hospital for a month to 6 weeks following his discharge from the inpatient unit for CODs. As in the past, Sondro has had a relatively uneventful inpatient stay. Once he gets back on his medications, regains physical strength, gets clean from cocaine, sleeps better, and feels safer, his paranoid ideation begins to diminish. He begins to engage with other clients; assumes responsibility for taking care of his physical needs; participates in group therapy on the unit; and, in general, appears contented. But the staff knows that when he leaves the hospital, he is at a high risk for relapse. He doesn't consistently take his medications, starts using crack cocaine, and loses his money and housing; particularly once he starts using cocaine, his paranoid ideation begins to manifest. The inpatient staff members, in consultation with the CMHC day hospital program staff and the ACT team, meet with Sondro to develop a comprehensive treatment and recovery plan. An essential part of this plan involves daily completion of a computerized check-in form, which monitors Sondro's functioning.
In this scene, Sondro is meeting with Irene, a nurse on the inpatient unit, and Mark, a member of the ACT team. Sondro has been active in developing his treatment and recovery plan, but he has some reservations about the computerized check-in process.
MARK: Sondro, we are all really excited about you, the inpatient and day hospital, and the ACT team all working together to create a really strong treatment and recovery plan for you this time. We really think this plan will make a difference in your recovery. I understand you have some concerns about using the check-in form, and we want to talk about that with you.
SONDRO: [after a brief pause] Yeah, I don't know about that.
MARK: Can you tell us a bit about your concerns?
Situations in Which a Check-In Process Can Be Particularly Beneficial
- Transitions from a higher to a lower level of care (e.g., from inpatient detoxification to an intensive outpatient program [IOP], from residential treatment to a halfway house)
- Periods of obviously increased stress (e.g., loss of domicile or intimate relationship, death of a loved one) with risk of relapse to substance use or exacerbation of mental illness
- Adjustments or alterations of medication for mental or substance use disorders
- Increases in a client's need for motivation and support to continue treatment (feedback on the client's own responses can be very useful)
- Repeated readmissions and difficulties in linking levels of care in recovery
- Introductions of new treatment methods or approaches not familiar to the client
SONDRO: Well, I just don't know about what you want me to do there in the mornings.
Master Clinician Note: Clients who express reservations about a technology-based intervention, as Sondro is doing, may be reacting to a combination of discomfort with using a computer, the introduction of something new into their daily regimen, and a manifestation of symptoms related to substance use or mental illness. For Sondro, part of what drives his reluctance is suspiciousness resulting from his paranoid illness. Staff members have already ensured that Sondro has basic literacy skills to handle questions on the computer screen, but it is worth noting that a lack of basic literacy skills can contribute to client resistance in situations like Sondro's.
MARK: Well, Sondro, why don't we work with you on this to help you get comfortable with the computer? You can try it out every day for the last few days you're here on the unit, and we'll have somebody right there with you in case you have questions. We can also maybe show you the computer you'll be using when you get to the day hospital. Would that take care of some of your concerns?
SONDRO: Well, I don't know.
MARK: I can understand that you have reservations. Is one of those that you worry about who might have access to the information?
SONDRO: Maybe a little.
MARK: I can reassure you that only the treatment team where you are currently in treatment—like right now, you're in the inpatient unit—and I will have access to the information. We do want to know how you're doing, and we especially want to be able to show you how much you're improving over time. The information you enter into the check-in form can tell us that.
SONDRO: So what kind of information does this thing collect?
How To Engage Clients With Automated Check-In Systems
To appeal to clients, there must be some noticeable benefit in the use of any type of automated clinical tool. The following strategies help increase the likelihood that clients will use and benefit from an automated check-in system:
- Encourage the client to tailor the information exchanged to his or her own recovery goals.
- Give something back. The benefits of one-way reporting to a clinician on symptoms may not be obvious. Helpful responses, delivered either in person or via automated messaging, should be tailored to the client's needs and desires.
- Allow the client to practice using the system with a staff member present to assist with the process and answer any questions that arise.
- Be clear and direct about the risks and benefits of participation, and encourage the client to make his or her own choice about participating.
- Engage peers who have found the system useful to help the client acknowledge benefits and practice using the system.
- Overcome equipment-related barriers by providing access to necessary devices, such as mobile phones, tablets, or computers.
- Use motivational interviewing to assess the client's willingness, plans to engage, and perceived obstacles.
MARK: Mostly, it's just information about how you're doing. For instance, we'll ask some questions about whether you're enjoying life, whether you're taking your meds, how your housing situation is going. We'll ask you about whether you're having cravings or feeling shaky about your recovery and whether you're having any symptoms, stuff like that. It takes about 10 minutes to complete, maybe a little longer until you get used to it.
SONDRO: Couldn't you just ask me the questions?
MARK: Well, we could, and we probably will continue to ask you some of them throughout the course of a day. But what we really want to do here is help you figure out where you're at when you feel the most comfortable, so when things start to go haywire, you'll notice, and you can kick up your wellness/recovery action plan. If you want, you can ask us to help you out, too.
There's one other thing that I didn't mention earlier. The questions on the check-in form are customized to you. Everybody who uses the program has the questions written specifically to address their needs. Of course, there are some that are the same for everybody, like, “How do you feel this morning?” But then there will be some questions for you about your housing, because that's been a problem in the past; about your disability money and whether it's secure; about whether you're taking your meds—things that you've said you want help with and worry about.
SONDRO: What if I get the questions wrong?
MARK: There aren't really any right or wrong answers—just your thoughts on how you're doing. And if you need help answering some of the questions, there will be someone available to help you. I think you'll see that it is really pretty easy and gives you time to think every day about how you're doing and what you need for that day.
SONDRO: Uh huh. What if I don't want to do it?
IRENE: Nobody's going to force you to do anything you don't want to do. We do believe this will be helpful, and we think you'll find it helpful, too, as we go along. But you have to give it a try if any of us are going to be able to see whether it works. A person will be there to help you with the computer and with completing the questions when you get to the day hospital.
MARK: So what do you think?
SONDRO: I guess I can give it a try. I'm a little concerned about people collecting data about me on computers.
MARK: I can understand that. Let me assure you that the information is for our staff—the people you know—and the only data are about how you are doing and what you have said you wanted us to help you with. For now, could you and I just give it a trial run? There's a computer here on the unit, right by the nurses' station, just for clients. I want to show you how to log in, access your own check-in form, work a keyboard, what kind of responses you'd put in, and so forth.
SONDRO: I can work a computer. I know how to use a keyboard. Just show me the form.
MARK: Okay, let's do it.
How To Help Clients Overcome Resistance to Computerized Check-Ins
Common points of resistance that clients have to computerized check-in include:
- Reluctance (shame, embarrassment) about using a computer because of a lack of exposure to the technology and training in how to use it.
- Limited reading skills or illiteracy.
- Ambivalence about recovery—about having their craving, substance use, and mental illness symptoms logged for clinicians to see and reflect back to them.
- Annoyance at being made to do something by someone they perceive as more powerful.
- General concern or anxiety about doing something new.
- Fear that the information provided will be used against them.
To overcome resistance to computerized check-in, you can use the same strategies you might use to motivate clients to complete paper check-in forms or other tasks:
- Help clients see the value of check-in so they will want to do it on their own.
- Help clients link progress toward one of their goals with the use of the program.
- Use motivational interviewing skills when starting clients on a new task.
- Work with clients to identify and overcome perceived obstacles to using the program.
- Emphasize the importance of collecting data for clients' well-being.
- Help clients feel like they are part of their own recovery teams by completing check-in.
Mark and Sondro do a trial run on the computer on the inpatient unit. Mark helps Sondro access the program and helps him create a username and password, and then Sondro completes the check-in process without problems. Sondro's username and password are stored by Mark in case Sondro forgets or wants to change them. Mark also emphasizes that Sondro needs to keep his password and user name secure and explains to him how to do so. The questionnaire takes about 12 minutes to complete. He does take some time to read the more detailed questions about drug use and asks Mark about one of the drugs listed (ketamine), saying he isn't familiar with it. Mark also asks Sondro to choose some questions that he would like to include in his check-in form from a list of optional questions. Sondro picks one about attending 12-Step meetings and another about physical exercise, two aspects of his relapse prevention plan that he has struggled to maintain in the past. A sample check-in form is presented in Part 2, Chapter 2, of this TIP.
How To Facilitate Client Computer Access in Treatment Settings
- Create private spaces where clients using computers can't be seen by rest of the client population.
- Provide trained staff members or peers to help troubleshoot.
- Make available written how-to sheets about operating the hardware or accessing support sites.
- Attend to Internet privacy and security standards by installing up-to-date virus, spyware, and malware protections.
- Protect client privacy by setting machines to delete cookies, search histories, and other private information that may otherwise be stored on the computer.
- Provide easily accessible links to support and education sites that you know are reputable.
- Block access to nontreatment sites to ensure that clients spend computer time on treatment-relevant activities rather than personal business (e.g., visiting social media sites).
- Offer basic computer classes taught by volunteers from the community.
- Consider firewall implications when using networked computers for client access to protect against unauthorized access to electronic clinical record systems or other confidential business applications.
Check-In Example
In a psychiatric inpatient and day treatment program in Western Australia, touchscreen access has been provided to clients participating in CBT groups. Clients complete the World Health Organization-5 Well-Being Index, a five-item measure of psychological well-being, each day. Therapists provide clients with a printout graphing their progress compared with expected progress and discuss results with clients in a weekly group. Therapists can use the well-being trend information to discuss treatment progress and realign treatment plans with their clients. An evaluation of the use of the touchscreen check-in demonstrated high levels of staff and client satisfaction with the tool, and client reports indicated that use of the technology increased their discussions with therapists about treatment progress and enhanced their understanding of their progress.
Sondro completes his inpatient stay without incident, filling out the check-in form each morning after breakfast. On the last two days of his inpatient stay, he works with a case manager to make the transition to a group home, where he will live for 3 months. After his stay in the group home, he will move to permanent supportive housing. Despite some distress about transitioning to the group home, he is compliant and shows no resistance in leaving the unit.
Part 2. Service provider collaboration
Mark meets Audrey, Sondro's primary counselor on the CODs day hospital unit. Audrey is not familiar with the check-in process and has questions about its efficacy.
MARK: Audrey, thank you for meeting with me today. I've gotten permission from Sondro to talk to you. I want to explain a little about the ACT team. Do you know what it is?
AUDREY: Well, we've worked with ACT teams before, but primarily as a referral resource when people leave the day hospital unit, so could you fill me in a bit?
MARK: Sure. ACT stands for assertive community treatment. It's a treatment approach that uses interdisciplinary staff members to provide community-based treatment and daily contact with clients, including services after hours. The team provides direct interventions to maintain stability of housing and entitlements and supports client compliance with prescribed medication regimens. When clients begin to relapse to drug use or mental illness, the team provides assertive treatment to reengage the client in recovery-oriented activities and family or peer support systems. Our ACT team is assigned to Sondro. I'm the case coordinator, but I want to emphasize that everyone on the team will be involved with Sondro's recovery. We'd like to work closely with you and your program to ensure that Sondro gets the best care possible from all of us.
Master Clinician Note: The privacy and confidentiality standards and regulations that typically apply to behavioral health services, including Title 42, Part 2, of the Code of Federal Regulations (CFR), Confidentiality of Alcohol and Drug Abuse Patient Records and the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule, also apply to electronic exchanges. As with any exchange of health records that are subject to 42 CFR Part 2, clients must provide written consent to share information across providers. Many states have laws that require consent for sharing information related to mental health. Offering clear, simple descriptions of the ways confidential information will be exchanged and providing a rationale for the exchange, along with an explanation of the risks and benefits associated with electronic information exchange, will help clients make informed choices about how their information is shared across providers and organizations. Providers must ensure that transmission of protected health and other confidential information is completed securely. See Part 2, Chapter 1, for more information on secure email and Web access.
AUDREY: That sounds great, and I look forward to working with you. Will you be involved with Sondro while he's here in the day hospital?
MARK: On an as-needed basis, yes. We want to collaborate on his care so that the transitions can be smooth and less traumatic. In addition to communicating with you and your staff, we also want to use a new tool that we think is especially useful for clients like Sondro, who in early recovery are particularly susceptible to relapse because of the combination of substance use and mental disorders. We have this computer-based program that'll help all of us facilitate Sondro's care. We don't want Sondro to disappear and then find out after a couple of days that he's begun using again or has been staying in a crack house. We want to find out early when he starts to lose momentum in terms of his recovery. The things that this program will track are the same things that you pay attention to: his participation in meetings, what his abstinence looks like, whether he's accessing intensive outpatient services and coming on time, how connected he is. It also tracks things that we look at in terms of mental health. Is he taking his medication? Is he having troublesome symptoms? Are the symptoms getting better or worse? You have a client computer that he can use here on the first floor, and every day, he'll check in. It allows us to go to the Web site and see how he's doing. This means that at the beginning of each day, even if we haven't asked about those things, we'll know how he's doing because the information will all be there. And there's another section of this site that will allow you and me to coordinate his care and communicate with one another.
AUDREY: Do you think he's actually going to tell the truth if he starts using drugs again?
MARK: We won't know for sure that he is telling the truth about every detail. But we'll also have some objective data in the mix—for instance, he is either using the check-in process or he is not. And we'll know if he checks in and says he is going to treatment, but you haven't seen him there. Then I'll know that, too, and I'll send someone on the team out to find him and offer him support.
Master Clinician Note: In general, studies of computer-assisted self-interview instruments demonstrate that clients are sometimes more forthcoming about sensitive, embarrassing, or shameful information when disclosing to a computer program than they are during in-person interviews (Islam et al., 2012; Richens et al., 2010). Web-based daily completion of check-in forms build on these studies by providing clients an opportunity to check in without talking directly to providers. A daily check-in process also provides a structure for collaboration between the client and the provider and a way for the client to be more actively engaged in recovery.
AUDREY: I don't see how this is any different from what I get from him every day. I see whether he is there, I analyze his urine screens, I observe his participation and see when he's getting upset. It isn't too hard to tell when people are getting sick again. Frankly, it just seems like another kind of paperwork.
MARK: I can see how it would appear that way, and no, we don't want to add to your workload. In fact, we think it will actually reduce it, eventually. This is a little more work on the front end; it's a change in routine as we're introducing a new treatment modality. The good news is that you can use the information from the check-in form in your clinical record keeping and reduce some of your charting. But more importantly, it's an opportunity for Sondro to participate in his recovery. Here's a printout of the check-in form we use. It's pretty comprehensive and, at the same time, pretty quick to complete. Your role in Sondro's care is still of the utmost importance, and your clinical judgment in determining how Sondro is doing will never be replaced. This is simply a tool to allow Sondro to play a greater role in his recovery and assist him with recognizing the warning signs that may indicate potential difficulties in his recovery.
Master Clinician Note: To support the client in repeatedly filling out the check-in form over time, the form must be relatively brief in length, take only a few minutes to fill out, and be meaningful to the client to sustain the motivation to complete it each day. The goal is to identify a few questions that are meaningful and important to both the client and the provider.
AUDREY: So I just have to pay attention to whether something is going wrong. What do we do when the data indicate that Sondro is headed for problems?
MARK: Well, first, we'll compare notes and get a better picture of what's happening. We can then talk with Sondro about our concerns and modify the treatment plan to better address the situation at hand. Our broad treatment goals for Sondro will always be to support his recovery from his substance use disorder; manage his mental illness; and help him maintain adequate family, housing, health, financial, social, and other supports that he needs to make it in the community. We both know it's going to be a long haul for Sondro, but I think the computer-assisted check-in process will be a great boost to him, especially in his early recovery.
Alternative Approaches for Conducting Check-Ins
- Voicemail or interactive voice response systems
- Mobile phone applications
- Secure Web-enabled tablets or personal computers
- Structured email
- Paper and pencil checklists entered into a computer tracking system
AUDREY: Are any of the questions on this check-in form going to be about his drug use?
MARK: Yes, he will be asked about things like cravings, slips, getting to his meetings outside of his IOP, if he is having any troubles there—for instance, with other clients, because you won't always be around to monitor him. Also, we can customize the form to include information specific to your program, information you particularly would like to have. In fact, we asked Sondro to identify the relapse risk factors that were most important to him, and he identified attending meetings and participating in his exercise group as areas he would like to track. The data the check-in form collects can help him see the connections between his symptoms and his behavior.
Master Clinician Note: The ability to customize the check-in form creates clinician buy-in by meeting the needs of their programs and also produces client buy-in, as clients can add items they identify as important metrics of their own recovery. Initially, it is helpful to ensure that support staff members also understand the program, can adequately answer client questions, and are supportive of their clients' use of the program.
AUDREY: Well, it sounds interesting.
MARK: Good. I don't want to lose sight of one of the things I consider most important. In terms of his recovery, this is a proactive act on Sondro's part every morning. He takes a greater stake in his recovery by completing this form. It's one more step in involving him in his own recovery.
AUDREY: You're right, and I'm willing to give it a shot. Maybe Sondro's case is a good one with which to try this out.
Part 3. Maintaining the recovery connection after IOP completion
Sondro is doing well, staying abstinent, taking his meds regularly, and has seen the ACT team psychiatrist at the CMHC for a medication check. His stay in the IOP was extended by 2 weeks to give him more time to stabilize. His contact with the ACT team has been primarily to support his IOP stay and to help him make adjustments in the community. The team is working with a local housing agency to help Sondro obtain permanent supportive housing in the community. In the meantime, he continues to live in the group home. He has regularly attended sessions at the IOP with only a couple of setbacks that were subsequently resolved. One occurred during a week when Audrey went on vacation; Sondro became suspicious and upset with the counselor who was leading the group for that week. The other occurred when Sondro got angry at another client in the group and refused to come back to the group for 2 days. With help from Audrey, he relented and reengaged with the group. After the first week of practice, completing his check-in form became a regular part of his day, and he reported that he actually enjoyed letting people know how he was doing. He felt proud to be able to report his progress and knew that both Mark and Audrey were aware of his reports. On a couple of occasions, Audrey used information provided by the check-in process as part of her ongoing monitoring and to give feedback to Sondro about his progress. Together, they charted trends and positive changes that Sondro had made.
Part 4. Sondro graduates from the IOP
Sondro has graduated and will not have day-to-day contact with the IOP staff any longer. Mark meets with Audrey about the recovery plan the IOP developed with Sondro, which includes checking in daily. Mark also introduces the idea of sending text message reminders to Sondro. These may be particularly important once he leaves the group home to enter permanent supportive housing in the community. Audrey will not be as involved because Sondro is no longer in her program. After a few months, if Sondro is doing well, the frequency of the Web-based check-in process can be reduced, but for now, the staff members of both programs think that sticking with the current frequency is best so as not to introduce another change in Sondro's life.
MARK: Sondro has graduated from your program and seems to be doing really well. Is that your impression, too?
AUDREY: I'm really happy for him. He has done well. He's still at high risk, and in just 24 hours, he can go right off the edge, but he'll be in our once-a-week continuing care group. If we see him getting shaky in his abstinence, we'll address that. If I think he is showing significant symptoms of mental illness, I'll call the ACT team. We can't enforce his attendance, but we expect that he will continue. He's been going to the Double Trouble in Recovery group that meets here every day, too, and we hope he will continue that, so we're really happy with his outcome. I have to say that I'm impressed at the data that we got back from the check-in process. We were really surprised. I didn't have much belief that it would make a difference, but it was nice for me to be able to get a quick picture, in a matter of minutes, of Sondro's functioning in a broad sense. I think the messages that appeared when he logged on to the system really helped him see that we were looking at the information and recognizing his positive progress.
Master Clinician Note: Double Trouble in Recovery is a 12-Step program for people with CODs. It is based on the 12 Steps and 12 Traditions of AA. Other programs, such as Dual Recovery Anonymous, may also be available in your area. Sometimes, the term “double trouble” is used to indicate that someone has a substance use disorder and also has a process addiction, or that someone participates in multiple 12-Step programs.
MARK: We'll still be monitoring and reinforcing his progress by having him check in. There could be a shift to a smartphone for the morning check-in process as he moves out into the community, but it will function in the same way as the desktop here at your program. Right now, the cost of a smartphone might be prohibitive for him, but in the future, the cost may come down. I'm also happy that he's willing to go to your continuing care and the Double Trouble group. I think we'll build in some reminders on the morning check-in process for Sondro about attending those meetings.
AUDREY: He's supposed to be going every day. Often, we find that he has trouble bonding in those groups, but we're going to support him in doing that. He seems happy there so far. I'm going to report to our administrator that we ought to do this check-in process for all our clients.
[Later, Mark meets with Sondro after his graduation ceremony from the day hospital program.]
MARK: So, Sondro, things seem to be working out fine. You're doing a great job.
SONDRO: Thank you.
MARK: You've had trouble for many years, and this time you really walked the walk. You're maintaining your abstinence, going to your outpatient treatment, taking your meds so the symptoms don't get in your way, and working on your physical health by participating in a walking group to get some exercise. I think you have a lot to be proud about.
SONDRO: That computer thing, it's pretty cool. It's not too hard and I like the color bars. When it's all green, I feel good. I like that when I finish, if I'm doing well, the bar turns green, and if I'm having a few troubles, it turns yellow. I haven't had but a few days where the bar was red, meaning I'm in big trouble.
MARK: That's the idea—for you to be in charge of your recovery. Checking in is one part of that, just like being in charge of keeping appointments, taking your meds, and being aware of times when you might need additional help. Audrey told me you now have a cell phone.
SONDRO: I do, but I'm worried that people can find me too easy.
MARK: Well, you don't mind us finding you, I hope.
SONDRO: No, you're okay.
MARK: Do you have text messaging on your phone?
SONDRO: Sure, but I don't know how to use it.
MARK: Well, if we show you how to receive your messages, how would you feel if we sent you text messages now and then—just little reminders? They'll help you stay on track. Do you think that might be helpful?
SONDRO: Well, if it's from you, I'm okay with that.
How To Talk With Clients About Using Technology in Their Care
Discussing the risks and benefits of using technology differs little from other discussions about changes to the treatment plan. Here are a few tips:
- Be honest. Don't oversell either the risks or the benefits associated with using technology. Discuss the ways the technology may be helpful and the risks associated with using technology as a tool.
- Honor and support client preferences. Ultimately, each client must decide whether to participate. It is a sign of recovery to make informed decisions about one's own life and treatment.
- Use change sampling. Allow clients to agree to a short trial of at least one aspect of a given technology-based tool or intervention, followed by a discussion of the experience and a renegotiation of consent to participate. It is helpful to demonstrate the use of the technology and then have clients try it in your presence to ensure that they are able to use it appropriately.
- Enlist peers. Other clients or past clients who have successfully used the technology can be effective champions and provide clear and honest feedback about the ways it helped or hindered their recovery experiences.
- Give back. No one likes to spend time doing something that has no personal payoff. Help clients identify the ways the technology might help them. If the benefit to clients is distant, find ways to enhance the incentives to participate.
How To Design Supportive Messages
Having a collection of brief messages to reinforce recovery can provide a quick and efficient way to help sustain motivation:
- Ask clients to help design and select the messages that are important to them.
- Tailor messages slightly to the circumstances of the client; for example, if you know that a specific holiday is hard for a client, send a message on that day or a few days prior, acknowledging the challenges and giving a tip for dealing with stress.
- Phrase messages positively—emphasize what can be done, rather than what should be avoided.
- Use peer support staff or peer counselors to send messages. These individuals can have a different type of credibility than professional staff members.
MARK: We'll send you text message reminders about ways to keep progressing and to give you a little push now and again. The messages won't include anything really personal; they'll just be reminders to do things or positive messages about your progress. We'll help you remember to take your meds, and we can text you as many times a day as you want. Does that sound reasonable?
SONDRO: Sure.
Master Clinician Note: Consider fine-tuning text messages for anniversaries, particularly those of stressful events, or to serve as reminders of specific appointments. Sending messages at a particular time of day or week to correspond to client needs can be helpful. If clients will regularly receive texts from you, you should be aware of their cellular plan costs for text messaging so that costs do not become burdensome.
MARK: We could send the text message at the times when you need it the most. What time of day is most difficult for you?
SONDRO: Six o'clock can be pretty tough. I have to be careful around then.
MARK: Well then, we will send your messages at six o'clock. Could you give me your phone number?
SONDRO: I could do that.
MARK: I'll check in with you to find out whether you think this is helpful. If it's not helpful, we can talk about it and stop if you want, or change it up to be more helpful.
SONDRO: What about the computer thing? The thing I do every morning.
Multiple Uses of Smartphone Apps
Kuhn et al. (2014) conducted a preliminary evaluation of PTSD Coach. Their focus groups with users/clients revealed the many ways in which the app was found to be helpful—learning about symptoms, managing symptoms, tracking symptoms, feeling one could do something about one's own posttraumatic stress disorder (PTSD), knowing when the symptoms were better or worse, accessing resources, overcoming prejudice and myths, providing a way to talk about experiences, and so forth. Clinicians and clients should consider all the possible ways to use apps.
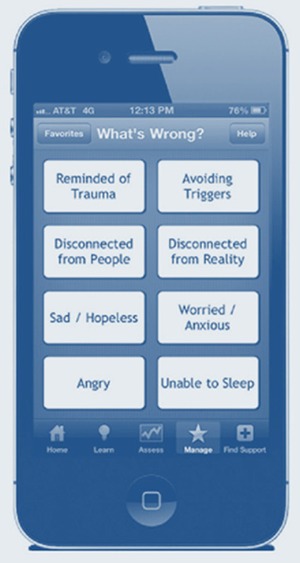
Master Clinician Note: Text messages are rarely secure or encrypted. Anyone with access to the client's cell phone can easily access his or her text messages. Even after they are erased, they may be accessible on the subscriber identity module card in the phone. Thus, if counselors use text messaging for reminders, support, or other purposes, they might want to keep messages vague and not reveal personal data. The client needs to provide specific informed consent related to the specific benefits and hazards of participating in online care. That said, the use of encrypted and secure communications as part of electronic health record (EHR) systems is growing rapidly. See Exhibit 1.2-1 for a research example.
Exhibit 1.2-1
Randomized Trial of Depression Follow-Up Care via Online Messaging. Simon and colleagues (2011) used their medical record system's capabilities to track prescriptions, make lab results viewable by clients, and allow clients to register for online messaging. (more...)
MARK: I think you should keep doing it for a while, because you're going through a big change now. Maybe soon we can arrange for you to do it from your phone instead. Would that be okay?
SONDRO: I like the computer thing. I like checking in every day.
MARK: You can use it every day for as long as you feel you need to.
SONDRO: Let's keep it like it is for now. I don't like change a lot.
MARK: Sounds good. Sondro, I just want you to know how proud we are of you and your accomplishments. You are really doing well. Keep up that good work.
Vignette 3. Conducting a Telephone- and Videoconference-Based Pretreatment Group for Clients With Substance Use Disorders
Overview
This vignette demonstrates how clients in a rural area who are on a wait list for treatment can be served by a pretreatment group conducted through video and telephone conferencing. Behavioral health programs in rural areas present some specific and unique challenges for service delivery. One of these challenges is limited access to care because of a widely dispersed population, geographic obstacles such as mountain ranges, travel expenses, accessibility of transportation, and frequent inclement weather. It is common in rural areas for clients to have to travel more than 100 miles to receive services. To address this issue, many programs have instituted a variety of telemental health services, using telephone, video conferencing, email, Web-based check-ups, and educational supports. Telehealth can be used for clients who are currently on wait lists and also as a primary tool. For example, Alaskan Native remote villages use telehealth as a primary healthcare tool; often, individuals go to the clinic in the village to access telehealth services delivered by a health aide or nurse.
Another issue facing many smaller programs in rural areas with a dispersed population is the wait time between when a client makes a decision to access help and when treatment services actually begin. This can range from just a few days to more than a month, depending on such issues as transportation, child care, employment, and an available treatment slot in either residential or outpatient services. In response, some programs have developed pretreatment groups conducted via telephone and/or video conferencing. Clients waiting to enter treatment are encouraged to use the group until other program services are available. This vignette depicts a pretreatment group that uses video conferencing on a secure network along with traditional telephone service.
Learning Objectives
- Identify circumstances in which telephone and video conferencing groups may be useful means of providing treatment and support for behavioral health concerns.
- Demonstrate skills in establishing and maintaining a supportive environment in telephone and video conferencing groups.
- Illustrate strategies for preventing or overcoming technological challenges when planning or facilitating telephone and video conferencing groups.
- Develop knowledge of the primary privacy, confidentiality, and anonymity concerns inherent in telephone and video conferencing groups, and learn strategies to minimize them.
Setting
Harry is a recovery coach assigned to lead a group that meets twice weekly at noon. He is fairly new on the job, but he has experience working in a group home where he ran groups before becoming a recovery coach. He was cofacilitator of the group for a month before taking over the leadership role, and Harry has now been leading the group for 3 weeks.
The first scene is a meeting between Harry and his clinical supervisor, Joanne. They go over the agenda for the group and the list of clients who will be participating. Joanne offers supportive advice on managing some issues that may arise in the group. The second scene is a group meeting attended by five clients. In this session, Harry uses an icebreaker that invites too much discussion and raises issues that cannot be addressed in the group. He also has to deal with a client who may be intoxicated. Prior to the next group, Harry checks in with Joanne and gets additional support and information. They specifically prepare for one client situation that may present a problem for the group. In the second group meeting, Harry must address a confidentiality issue.
Harry's Story
Part 1. Meeting with a supervisor
Harry meets with his supervisor, Joanne, shortly before meeting with the group. He and Joanne cover some of the basic objectives of the group, the group format, the ground rules for participants, and concerns Harry has. Joanne, who has experience with telephone-based and video conference-based counseling, works with Harry to help him manage any glitches that might arise.
HARRY: I think I'm pretty well set up for the group today at noon. We have five participants.
Dee, who is in her third week in the group, is trying to arrange child care for when she's in intensive outpatient care. The problem is that her husband is a truck driver and on the road for up to 2 weeks at a time. In the meantime, she is attending online AA meetings, has a sponsor, and is going to two AA meetings a week in her community. She's been clean now for three and a half weeks. I'm concerned about her losing her motivation for treatment. She uses her computer to access our video conferencing system to attend the group.
Bobby—he's 26 years old—was arrested about a month ago for driving under the influence of substances, did 25 days in jail, and is now out on the condition from the court that he enrolls in treatment. He was in the center last week for assessment and is third on the list for an inpatient bed. It's going to be tough for him to stay sober outside. He lives way out in the country with his parents, and what's keeping him sober right now is basically having no driver's license and no way to get booze. He accesses our services via telephone through our secure video conferencing network.
Gene first connected with our program about a year ago and has a long history of pain pill addiction and alcohol and marijuana use. He is a disabled veteran but comes to our center because the closest service center available through the U.S. Department of Veterans Affairs (VA) is so far away. Lately, he's really been struggling. We have him scheduled for our ongoing recovery group. He only lives about an hour away and thinks he can make it for the weekly group. He's accessing the group through the video conferencing system.
This will be Mary's first group. She was just in yesterday. She's a widow—her husband died a couple of years ago, and she manages a ranch that she and her husband owned. The kids are all grown and have moved away, but they've gotten increasingly more concerned that their mother is getting drunk every night. Last week, she was drunk and called her daughter, who lives in Minneapolis, and started talking about not being able to go on, and how the ranch was too much, and how much she missed her husband. She scared the daylights out of her daughter, so the kids all came in last weekend and did their own version of an intervention. The youngest son, who's on break from college this month, is staying with her for now and brought her to the center yesterday. She'll start in the IOP next Monday. We also have her scheduled for a mental health consultation next week to get a measure on her depression. She's never used video conferencing before, but her son will set it up for her on his laptop and get her started.
That leaves Morris, who only attends the group about half the time. I'm assuming that when he doesn't, he's drinking. At least, that usually seems to be the case. Morris just really resists treatment, but is amenable to at least participating in the group and staying connected to us that way. He calls in via telephone through our secure network. He lives here in town and would probably be a good candidate for our IOP. Every time we get him in, though, he finds a way to sabotage it. He pretty clearly has some mental health issues, maybe involving PTSD, that scare him away from treatment. Our goal is just to stay connected with him and maybe help him move from precontemplation/contemplation to actually getting in treatment. But, if we push, he just runs away.
JOANNE: Well, what an interesting group of people. Pretty diverse. But, you know, all of these folks are going to get some help today because of our video and telephone outreach. Otherwise, they wouldn't keep in contact with us, and we'd have no sense of how they were doing. This is a valuable program. It not only offers people some immediate help, but also keeps them connected to us until they can enter more formal treatment.
So, you're comfortable with the format? Two people are going to be telephoning in; three will be on video. The group lasts about 45 to 50 minutes, sometimes a little longer. We're not doing treatment, just preparing people for treatment—helping them maintain momentum, providing some education. Many of the folks in these groups have recently moved from precontemplation to contemplation, or from contemplation to preparation, and we want to help them hold on to their new outlook and goals.
Everyone will be connecting through our secure and encrypted video conferencing network. They know that they'll hear and not see each other, but that you'll be able to see all of the folks that are accessing via video, and, of course, the ones with video can see you. Each participant will have signed an informed consent form prior to joining the group, which can be done in person or through an online document signature system.
HARRY: I've had something of a problem with clients interrupting each other. It's not my style to be too directive, but I've learned to call on folks who aren't saying much and, on a couple of occasions, I've had to ask someone to wait until another person finishes talking. It seems like, for most people, after a while they learn to pause until there is a break in the conversation.
JOANNE: I think it's easier when all clients can see each other, as it is in our long-term recovery video group. But here, for confidentiality reasons, clients only see an avatar of other clients.
Master Clinician Note: An avatar is an icon, picture, character, or graphic that represents a person's online identity. Using an avatar allows a person to portray an online identity without revealing their real image. In most situations, the counselor can see each client via the video feed, and each client can see the counselor, but clients do not see actual images or video feeds of the other participants.
Comparison of Use of Telephone Versus Video Conferencing
| Advantages | Disadvantages | |
|---|---|---|
| Telephone |
|
|
| Advantages | Disadvantages | |
| Video |
|
|
JOANNE: Now, the usual flow of the group is that you begin with a check-in and maybe give people an icebreaker, just to help them get started. I think the one you used last Thursday was great: “The best thing that has happened to me today is…” You want to just get a feel for how people are doing, whether there are any crises and special problems that need to be addressed. Of course, if the problem is unique to them, or serious, you'll want to let the person know you'll be following up with them after the group ends. Early on, you want to get everyone engaged in the discussion. I also find it useful to go over the ground rules quickly with every group.
HARRY: In the other groups I've run, I've found it's best to let the initial interaction run for maybe 10 to 15 minutes. By then, I'll have a feel for how people are doing and whether there are any pressing needs. I will have been able to invite quieter people to get involved and to set the tone for the session. Then, for the educational part of the group, Willie, from the IOP, is going to come in and talk a bit about that program and how it operates.
Ground Rules for Pretreatment Telephone or Video Groups
Most of the rules applying to in-person groups are also important in telephone and video conferencing groups; however, some issues become magnified when group members are dispersed. The following rules help minimize issues that can arise in telephone and video conferencing groups:
- One person talks at a time.
- For conference calls, callers say their names before they speak, because callers might not recognize each other's voices.
- Everyone has an opportunity to talk.
- Everyone should minimize noise and other distractions during the group and use the mute button if needed.
- No one other than the group members and leader should be viewing or listening in unless they have permission from the group leader and the group is aware that someone else is participating.
- Participants are encouraged to control disclosure of their identities to others in the group by using only first names and avatars rather than their real likenesses or surnames.
- Indepth or highly sensitive discussions between clinicians and clients should be scheduled outside the group setting.
- The same group rules related to respect, honesty, and confidentiality used in in-person groups also apply to video and telephone groups.
As you know, Willie can talk from both sides of the fence, as both a counselor and a client. He does a great job of helping people develop hope that things can get better and that recovery is possible. He's also great about getting people to ask the right questions: “What if I know somebody in the group,” “What if I need to miss a session,” “What happens to confidentiality if my cousin works for the mental health center,” “Can she read my records,” those sorts of things. His confidence about recovery inspires people who may still be on the fence about treatment.
JOANNE: Well, Harry, it sounds like you're about ready to go. Now, you know if you have a problem, all you have to do is buzz me and I'll come right in. Sometimes, people need to be taken off the group for a while, and I'll handle that for you if it comes up. If somebody is creating a problem for the group, or if you need some support, just let me know.
Master Clinician Note: When doing treatment groups with clients who are not all physically present in one room, it helps to have a backup person or a cofacilitator who can assist when a client becomes disruptive, has emergency needs, or exhibits some other pressing issue that needs to be handled individually, away from the group. In working with clients on the telephone, this may mean establishing a new call between the backup counselor and the client in crisis. With video conferencing, there should be arrangements to redirect the connection of the client in crisis to a separate, private monitor staffed by the cofacilitator.
HARRY: Sure will, Joanne. Thanks for the support.
Part 2. The group meeting
Harry signs into the secure network about 10 minutes early. The first to call in is Morris, who has attended this group before. He and Harry chat for a bit, waiting for others to arrive. The next to arrive are Mary and her son. Once Mary is established online, the son leaves his mother alone in the room. Harry speaks briefly with Mary, who isn't very communicative. Harry has a video connection with Mary and observes that she seems anxious. Dee arrives soon after Mary. The microphone on her laptop seems to exaggerate the noise of her children playing and the sound of the television in the next room. Harry asks Dee if she would feel comfortable shutting the door to the next room, and she obliges. Right at start time for the group, Gene appears onscreen. He looks disheveled, like he just got up, and is drinking coffee from a large mug.
HARRY: Okay folks, it's time to start, and we have Morris, Mary, Dee, and Gene attending. There may be one other person joining us, but let's begin.
MARY: Am I supposed to be able to see all these other people? I can see me and you, but I only see silly pictures of the others. On Skype, when my son sets me up to see my grandchildren, we all see each other.
HARRY: Actually, Mary, in this group, what you see on the screen are avatars, or images representing people. For this group, we do that for confidentiality reasons, and because some people are calling in via telephone. So, I can see you and you can see me, but the group members can't see each other. Unlike with Skype, we use a special teleconferencing network that you call into on your computer. It's a secure network that ensures confidentiality.
MARY: Thank you.
HARRY: Okay, let's start with folks giving their first names, and maybe each of you can say a little bit about yourselves and let us know how you are doing.
MORRIS: Well, I'm Morris, and I come to the group when I'm not busy with other stuff.
DEE: [after a pause] Well, I'm Dee, and I'm a housewife outside of Seradona. I have three kids who are out of school today, and you'll probably hear them in the background.
MARY: [after a pause] I'm Mary, and I own a ranch outside of town. My husband died last year, and my kids think I'm drinking too much. I don't see how this is going to help me. I'm already too overloaded and have too much to do, and now they want me to do this silly thing. Sure, I drink, been drinking all my life. But I don't get looped and I don't drive drunk, so I don't even know why I'm here. Running a ranch is hard work, and keeping up with a bunch of cowboys is even tougher. My husband used to take care of that. Now he's gone, and I'm stuck with it. Am I talking too much? Just tell me to shut up if I am. I'm just frankly pissed that I have to do this.
Technical Considerations for Video and Telephone Groups
- Use a secure teleconferencing network or land-based telephone conferencing system to protect privacy.
- Consider adequate bandwidth at provider and client ends of the transmission to facilitate adequate image resolution.
- Anticipate fluctuating bandwidth demands when relying on public Internet.
- Address the need for encryption of information on provider and client ends of transmission to ensure privacy. Depending on the service, this may require software to be downloaded and set up by the client.
- Test audio equipment to troubleshoot inadequate audio quality. Choose technology that can run on very low bandwidth if possible.
- Ensure that your technology allows you to mute or remove disruptive members in the group.
- Provide a land-based telephone line for backup.
- Ask clients to test the system prior to the group meeting time.
HARRY: Thanks, Mary. Maybe we can get back to this in a minute. Let's hear from Gene.
GENE: Uh, I'm Gene. I just got up. I don't sleep at night, so at three o'clock this morning I finally took a sleeping pill, and it knocked me on my butt. Now it's noon, and I'm hardly awake.
HARRY: Well, Gene, and all of you, I'm glad you've joined us today. I'm Harry, and I'm the leader of the group. My job here at the center is to work as a recovery coach. I work with people who are thinking about changing their alcohol and drug use, run some groups, help people make connections in the community for recovery needs like healthcare or financial assistance, and just try to help people get started in recovery. For those who are new to this group, I'd like to start by describing the purpose of this meeting.
[Harry proceeds to describe the rules of the group briefly. (For more information on group rules, refer back to the “Ground Rules for Pretreatment Telephone or Video Groups” box earlier in this vignette.) Harry also explains the goals of the group, stating that the group is one of the program's online resources and that clients who take part are often doing so to receive some assistance without always having to visit the agency. Assistance can include information that comes from Harry, from other clients who are part of the group on the call, or from other staff members or workers from outside the agency who attend the group sometimes to address certain specific issues.]
HARRY: The goals of this group are to gain assistance from each other as well as from the group process itself; for those who are new to the group, some of its workings will become clear as the group process unfolds. If there are any questions at any time, just let me know. So, let's begin with me asking you to think about something for a minute. If you could have anything you need at your disposal today, what would you like to have?
MORRIS: I don't understand. Is this a test or something?
HARRY: No, I'm just wondering what you might need in your life today—what would help you live a better life today?
DEE: Well, I know the answer to that one right away. I need my husband to be home more. He's a long-haul driver and does cross-country runs for 12 consecutive days. Then he's back home for 4 days and sleeps most of that time, and then he's on the road again. So, it's like I'm a single mom almost all the time. I know he gets lonely too. He calls me a half dozen times a day, telling me where he is and what the conditions are like. It's a boring job. We live a pretty good ways from town, so when the school bus picks up the two older kids and it's just me and the baby here at home, there's not a lot to do but answer the phone and drink a few beers. Then he gets upset when he calls ‘cause he can tell I'm drinking, and then we both get upset, and I just have another beer. I'm doing okay today, though. It's just past noon, and I haven't had a beer yet.
[Harry quickly considers the options of where to head at this point. This is not a treatment group, but Dee is clearly asking for support. On the other hand, if he ventures into working with Dee, he might leave other group members feeling disengaged. If he invites other group members to engage with Dee to support her, he will have drifted from the agenda of the group, and the other group members will probably just get into giving advice. He decides to briefly support Dee's efforts to resist drinking and makes a mental note to get back to Dee for an individual video session later this afternoon.]
Master Clinician Note: Just like in any group, it's often tricky in telephone and video groups to deal with individual issues while keeping the whole group engaged. If group members cannot see each other, they are even more easily disengaged from these exchanges. Communicate to the individual that you support his or her struggles and will have time to talk individually about the situation later. Once this has been accomplished, you can reinitiate group interaction.
HARRY: Dee, congratulations on not drinking today. That's a good step in the right direction. I'm wondering if we can talk briefly at the end of group today about the issue you raised. Would that be okay?
DEE: Sure.
HARRY: Okay, that's great. What might the rest of you need, if you could have whatever you want today?
[With Harry's support, each group member contributes to the discussion, describing his or her needs. Gene, who has chronic pain, would like pain relief. Mary would like her husband back, alive and running the ranch. Morris would like some friends. Harry briefly suggests that Morris might make some friends in the treatment program if he is willing to attend, but Morris rejects the idea. Harry has hints of regret that he used this particular question in this group. His objective was to get everyone involved, but it ended up raising issues that could not really be discussed and resolved in this kind of group. Harry does encourage Gene to raise the chronic pain issue with his counselor at the center and to make that a particular goal for his treatment. He also encourages Mary to talk about her need for support with her son and to begin making plans with him and her other children for getting some help in running the ranch.]
HARRY: Let's move on now to our special guest. We've invited Willie from our IOP to talk with us today. Willie, I want to welcome you into the group. On video, we have Mary, Dee, and Gene. On the phone, we have Morris.
WILLIE: Good afternoon, everyone. I'm delighted to be here today to tell you a bit about the center's IOP, to talk a little about treatment and recovery in general, and to answer any questions you may have.
Willie proceeds to describe the IOP, interacting with the four group participants and, in particular, describing his own experiences with recovery and using them as a framework for helping clients begin to consider their own expectations, through group discussion, about what recovery might be like for them.
In the meantime, Harry has gotten a notice on the monitor that someone else is trying to enter the conference. He steps into Joanne's office and answers on her telephone. The call is from Bobby, the group participant who did not check in with the group this morning. While Willie continues to direct the group, Harry speaks with Bobby alone. Bobby seems to be intoxicated; he is slurring his words, rambling, and making different excuses for being late for the group. Harry asks Bobby if he has been drinking. Bobby deflects the question and continues to ramble about why he is late for the group. Harry does a quick clinical assessment of Bobby, checks that he isn't a high risk for suicide, and gives him a suicide hotline number. He also offers to help Bobby make arrangements to enter detoxification, which Bobby declines, and checks Bobby's plans for the day to ensure that he isn't driving. He closes the call by asking Bobby to call in the morning, when Harry thinks it's less likely that Bobby will be drinking.
After making arrangements with Bobby to call the next morning, Harry returns to the group. As Willie wraps up his presentation, Harry becomes more engaged in the group process and thanks Willie for his participation. Harry then invites group members to comment on what they have gotten from today's discussion. Harry mentions that he talked to Bobby offline during Willie's presentation and hopes that Bobby will be able to attend group on Thursday. He reminds Dee of their telephone appointment at 4:00 p.m.; encourages all participants to get or stay engaged in a 12-Step program or other mutual-help group in their area or over the Web; reminds them that if anything comes up that they would like to discuss, they can feel free to give him a call; and closes the group with a reminder of the next group meeting, which is Thursday at noon. He will email each group member a reminder of the Thursday meeting.
Following the group meeting, Harry drops into Joanne's office to get her thoughts about handling the issue of Bobby being intoxicated and Harry not letting him join the group. Joanne agrees that inviting a person who is probably intoxicated into a group of people in early recovery would be detrimental. Harry was careful not to be judgmental with Bobby about his alcohol use, but, at the same time, firm in not allowing him to participate in the group while intoxicated. Harry also made an appointment for Bobby to call at 9:00 a.m. tomorrow and discouraged drinking in the interim.
Part 3. Supervision
In supervision later in the week, Harry and Joanne meet to review the group process and discuss Harry's concerns about the group meeting. Bobby did not call after the group. Harry plans to telephone him on Wednesday to remind him of the group meeting tomorrow at noon. Dee kept her 4:00 p.m. appointment and arranged a video conference session with a counselor on Friday. In the interim, Harry encouraged her to employ a neighbor's teenage daughter to babysit while she goes to an AA meeting in her local community. The small AA group only meets twice a week, but it gives Dee a chance to meet some people in recovery and get out of the house. Dee also reported that her husband strongly supports her efforts to quit drinking and get help. Harry and Joanne go over plans for the group tomorrow. The guest is going to be a local AA member who will speak briefly about opportunities to attend AA and other 12-Step and support meetings in the community and online. Harry is going to give more thought to the questions he asks to get people involved in the group, and he will try not to ask questions for which there may be potentially complicated answers that cannot be addressed adequately in the brief group setting.
Locating Online and In-Person Mutual Support Groups
Online and in-person mutual-help groups can be important resources for clients participating in telephone or video conferencing groups. A range of mutual-help resources are available online. Although some clients will be very sophisticated users of social media, others will need advice about how to protect their privacy when using social media. See Part 2, Chapter 2, for a link to safety tips for social networking. The following resources may help you select reputable mutual-help groups:
- Substance Abuse In Brief Fact Sheet: An Introduction to Mutual Support Groups for Alcohol and Drug Abuse (http://store.samhsa.gov/product/An-Introduction-to-Mutual-Support-Groups-for-Alcohol-and-Drug-Abuse/SMA08-4336)
- Faces and Voices of Recovery: Guide to Mutual Aid Resources (http://www.facesandvoicesofrecovery.org/resources)
Part 4. The second group meeting
Harry opens the televideo meeting space about 10 minutes before the group is scheduled to begin. Mary is the first to check in, but she cannot be heard because she has pressed the mute button on her computer. Harry quickly calls her home telephone number and helps her activate the speaker on her computer. In rapid order, Morris (telephone), Dee (video), Gene (video), and Bobby (telephone) come online.
HARRY: Welcome, folks. We have everyone who is scheduled to be here online. Morris and Bobby are connecting with us by telephone.
A loud screech can be heard in the background. Harry's console indicates that it is coming from Bobby's telephone.
HARRY: Bobby, there might be a problem with your phone. Are you on a cell or landline?
BOBBY: I'm driving to the store and I'm on my cell. I gotta get to the store and cash my check and get some cigarettes.
HARRY: [trying not to show exasperation] Bobby, I appreciate you making the effort to connect with us today; that is, for sure, a step in the right direction. However, I am concerned that you're driving while on the phone. Can you put the phone down, find a safe place to park, and then pick the phone back up? We won't hang up; we'll wait for you. If not, would you give me a call this afternoon when you get back home, maybe around two o'clock? Would that work for you?
Master Clinician Note: Although land-based telephone connections tend to be slightly more stable than cellular connections, it is no longer realistic to require clients to access telehealth services through land lines only. Many people do not have land lines in their homes anymore and rely solely on their mobile phones for telephone-based communications; public payphone landlines are less and less common and are often in highly trafficked locations that might well compromise client confidentiality. Security issues to consider when using mobile phones are addressed elsewhere in this chapter. As for connectivity issues and reception-dependent quality of audio and video transmissions from clients using mobile phones, you may consider asking clients to try out various easily accessible locations prior to accessing telehealth services so that they can select a location with adequate, stable reception. They can then plan to be, and remain, in that location for the duration of their participation in telephone-and/or videoconference-based behavioral health services.
How To Manage Challenging Interactions in Telephone or Video Group Meetings
- Have a backup clinician help with crises or difficulties as you continue with the group.
- Encourage the use of appointments outside the group session to address sensitive issues.
- Do quick status checks with each participant to identify any issues that need to be addressed either in group or after the group.
- Establish clear group rules and norms in the beginning; reinforce them during each session.
- Consider practicing your protocols with a peer before your first session.
- Use structure (e.g., check-ins, topical discussions) to ensure that everyone has a chance to talk.
- Have resource lists available to provide referrals quickly.
BOBBY: [defensively] Well, man, I gotta get my check cashed and I'm outta smokes. Sometimes you just gotta do what you gotta do.
[Bobby hangs up. Harry is concerned that he is talking with a person who is probably violating the law by driving without a license; Bobby's was revoked for driving while under the influence. Harry will consult with Joanne as soon as the group is finished to see what he should do. He is also aware that the rest of the group was listening in on the interaction.]
MORRIS: Well, I'm glad you got rid of him. I don't like him.
DEE: He kind of gives me the creeps.
GENE: Well, I think the guy is just doing what he's got to do.
HARRY: Guys, I'm concerned that we're going to sit here and critique Bobby. Instead, let's move on to our agenda for the day. Suppose we start with a check-in. How about checking in by giving us your first name and what you would like to get out of today's meeting?
DEE: Well, I'm Dee, and I want to let you know that I did hire the neighbor's girl as a babysitter, and I went to a meeting in town last night. It was only six old guys and me, but you know what? They were friendly, and I felt welcome, and they invited me to come back. I wouldn't say it was a good time, but it was nice to get out of the house, and I felt welcomed at the meeting. One of those guys got sober before I was even born. Can you imagine? Somebody hasn't had a drink in 34 years! He was a hoot. I'm surprised he can even remember back then.
MARY: Honey, some of us aren't as slow as we look. I'm pushing 70 and I still run a ranch!
HARRY: Mary, introduce yourself and tell us what you would like to get out of today's meeting.
MARY: Oh, sorry. I'm Mary, and I don't know what I need to get out of this. I guess what I need to get out of this is to get out of this. My kids put me up to it. Forced me, actually, and it looks like they're going to stay on me until I cut back on my two or three drinks in the evening. You know, there isn't much to do on the ranch after about seven o'clock at night.
HARRY: Okay, so what you would like to do is complete the program?
MARY: I guess that puts it pretty clearly.
Master Clinician Note: Notice that rather than fighting resistance, Harry asks Mary to identify her own goals for participating. This can be an effective way to create ownership for change. Asking clients to identify what they want helps to refocus them on their own goals rather than on goals others may have for them.
HARRY: Okay, who else is here?
MORRIS: Well, I'm Morris. I just want to say… Dee, I figured out, you being from outside Seradona and all, that I went to school with your sister, Jan. Actually, I had a crush on her, but she wouldn't go out with me. I think you're a little older than her, and you married Billy Rogers and then y'all got a divorce, right? [after a long silence] Did I say the wrong thing?
HARRY: Well, Morris, I think we want to help people keep their anonymity here, to preserve people's confidentiality, you know. That's why we only use first names. You might, particularly in a small place like where we live, figure out who some group members are or who they're married to. But I think it's always wise to let them decide what to share and what they want people to know about them and their personal lives. Otherwise, it can feel dangerous, kind of like they're being exposed.
MORRIS: Well, I was just trying to be friendly.
HARRY: I understand that. I don't think you were trying to expose anyone intentionally. Dee, you have anything to say about what's happening?
DEE: Yes, I know who you are. I think I'd rather you not be talking about me in the group, but I don't think you meant anything mean by it. So, let's just forget it—especially the part about Billy Rogers.
MORRIS: Well, I'm really, really sorry.
GENE: Could we just move on here?
[Harry begins to think he is getting in over his head, but he doesn't think it would be appropriate to call Joanne in. He does make note of items to discuss with Joanne after the group.]
HARRY: Gene, you're the last check-in. What would you like to get out of today's meeting?
How To Manage Confidentiality During Telephone or Video Group Meetings
- Review privacy and anonymity guidelines with each client before they join the group and again as a group whenever new members join.
- Help clients differentiate between anonymity and confidentiality; honor both in the group.
- Mail or email a confidentiality statement/agreement to clients before the group begins.
- Remember to cover traditional confidentiality and anonymity concerns as well as those that are unique to telephone and video groups, such as other people entering a room when a group member is online.
- Distribute a sheet of safety tips about Internet privacy and risk to clients at the time they enroll in group (see Part 2, Chapter 2, for links to sample safety tips).
- Connect clients with options for online support that do not compromise privacy, such as mutual-help groups, chats, and blogs.
How To Get Assistance During Telephone or Video Group Meetings
When scheduling telephone or video groups, plan for backup support to help manage unexpected situations. Ideally, support will consist of a second clinician who is on call and technology that allows this clinician to take a client into a separate discussion if necessary. Remember to:
- Let the group know what is going on. They may not be able to see, hear, or detect concerns as you can. Tell them if you need to exit the group and how long you expect to be gone.
- Deescalate the situation by offering individual support from another clinician or by offering to engage with the client one-on-one after the group. Schedule a follow-up session immediately after the group, if needed.
- Avoid disclosing personal information about any individual in group. Stick to statements like, “It sounds like you could use some extra support,” or, “Let's talk more about this after group,” which communicate to the other group participants, without disclosing additional information, that you are planning to follow up with the client in need.
GENE: Well, I'm Gene. And I called in today especially because I'm feeling pretty shaky. I'm craving bad. I've really tried not to take the pain pills for a couple of days now—three, actually. I've smoked some, but no booze and no pain pills, and I'm beginning to feel my skin crawling. Like I'm itching.
HARRY: Gene, I'm wondering if you think you need to talk to someone now about coming into the center. Sounds like you may be having some withdrawals.
GENE: Damned right I'm withdrawing. Man, I need something.
HARRY: Okay, right now, let me put the group on mute for a minute and I'm going to make a phone call and see what we can do.
[Harry mutes the group and calls Joanne. Joanne answers and agrees to take Gene offline, do a quick evaluation, and arrange for any care he may need. Harry returns to the group and unmutes his line.]
HARRY: Gene, I'm going to switch you over to Joanne. You may remember her from your evaluation session here at the center a couple of weeks ago. She's going to talk with you personally, and the two of you can make some decisions about what needs to happen. Is that okay with you?
GENE: That sounds about right.
HARRY: Okay, everyone. Hold on for a minute while I mute the group and help Gene get connected to Joanne; I'll be right back with you after that.
[Harry connects Gene and Joanne, makes introductions, and then returns to the group, unmuting his audio feed once more.]
HARRY: Okay, everyone, I'm back. Next, I want to introduce our guest this morning, Michael, who is a graduate of our program and a person who is active in mutual-help groups in the community. Michael, welcome to the group.
How To Manage an Exchange of Personal Information in an Online Group
Clients may wish to exchange personal information for a variety of reasons. Clinicians can help clients manage their privacy in the following ways:
- Review guidelines for anonymity regularly in groups and individually.
- Distribute information about how to control access to private/identifying information before the clients participate in online interactions.
- Take clients temporarily offline to reinforce privacy when needed.
- Support out-of-group discussions through chats, blogs, and other mutual-help options.
- Facilitate talks among participants who wish to share personal information as needed.
- Invite guest speakers to discuss Internet privacy concerns and protections.
[Michael introduces himself and talks about his experience in mutual support groups in the area. He answers several questions about anonymity in the groups, groups for women, relapse, and other topics. After about 15 minutes, he turns the meeting back over to Harry.]
HARRY: Well, folks, I think that about takes all the time we have for today. Before we stop, are there any closing questions or comments?
MORRIS: Dee, I still feel terrible about what I said. I only meant to see if you were Jan's sister.
DEE: No problem.
HARRY: Dee, I'm wondering if you and Morris would like to meet for just a few minutes after the group is over for you guys to clear the air over anything left over from today?
DEE: I really don't need to.
MORRIS: Me either. I feel bad about saying what I said, but I'm glad Dee isn't upset with me.
Harry closes the meeting, reminding people about confidentiality of information the group shares, about the time for the next group meeting, and about calling him or other staff members if they have questions or if something comes up for them over the weekend. Harry has also kept a list of items that he needs to discuss in his next supervision session with Joanne. He remembers that Bobby is supposed to call around 2:00 p.m. and makes a mental note to await the call.
Vignette 4. Incorporating TAC Into Behavioral Health Services for Clients Who Are Hearing Impaired
Overview
TAC offers a variety of previously unavailable options for individuals with special needs to access treatment. These special populations include people who live in rural and remote areas, people with disabilities that limit access, individuals whose employment limits their options for regularly scheduled services, and people who will not access services through conventional (e.g., office visits, in-person counseling) methods. Additionally, TAC opens up the possibility of maintaining contact when not in session by using motivational messages, simple wellness check-ins, appointment reminders, and other options.
Some individuals who are hearing impaired consider themselves part of a community that, in fundamental ways, has its own cultural identity; individuals in this community prefer the term “Deaf,” which does not directly reference impairment. To promote cultural competence, the counselor in this vignette follows the client's wishes and uses the terminology most conducive to recognizing and respecting the client's cultural beliefs and identity. In all other areas of the TIP, the term “hearing impaired” is used to refer to individuals who are Deaf or hard of hearing, but in Vignette 4, the terminology reflects the preferences of the Deaf community.
This vignette describes ways in which technology can support intake, assessment, referral, treatment, and continuing care for Deaf clients, a specific group of people for whom technology plays an important role in access to care. It also addresses ways in which Web-based technologies and supports can help deliver behavioral health services to the Deaf population. The use of computers, smartphones, and other Internet-supported devices enables users to have in-person conversations as well as typed and video-based communication in real (synchronous) time. In addition, some recovery resources, once only available in print form, can now come to life in American Sign Language (ASL) for Deaf users. The 12 Steps, daily affirmations, and other valuable tools are now available for Deaf consumers in video form and can be viewed via the Web.
Setting
The county behavioral health agency is located in a small city and provides outpatient services to residents who may live as far as 30 miles away. The agency provides accessible services to clients with disabilities, including Deaf individuals seeking help. There is no one on staff, however, who is fluent in ASL or has extensive knowledge of culturally appropriate treatment for Deaf clients.
Learning Objectives
- Identify how TAC can enhance accessibility and treatment for Deaf clients.
- Explore special considerations and options for treating Deaf clients who have mental or substance use disorders.
- Understand a variety of accessibility issues in providing services to Deaf clients and how TAC may be an avenue for addressing these issues.
- Learn privacy and special counseling considerations when using TAC.
- Learn how to use Web-based supports to enhance client outcomes.
Maria's Story
Part 1. Beginning to work with an interpreter
Maria is a staff counselor at the county behavioral health agency who had some experience working with Deaf clients during her internship in graduate school. Her new client, Mike, is a 32-year-old Deaf man who has been referred to Maria's agency by the court for substance use disorder assessment. Maria makes a few calls and does some Internet searches; she learns that there are a few different treatment options for Deaf clients. One is a mainstream program using an interpreter in a local agency with inpatient and IOP options, both designed primarily for clients who can hear. Another option is for the client to attend a specialized treatment program that is linguistically and culturally appropriate for a Deaf client, with staff members who are able to communicate directly in ASL. For example, the Minnesota Chemical Dependency Program for Deaf and Hard of Hearing Individuals (MCDPDHHI) in Minneapolis, MN, accepts clients from across the United States.
Considerations Prior to Your First Session With a Deaf Client
- ASL will require a certified interpreter who is competent in the language of the client.
- Interpreter referral services are sometimes administered through the state by an outside agency or through a contract with the state. Payment of interpreters is typically provided by the agency if they are required by law to provide accessible services under the Americans With Disabilities Act.
- A client may choose not to work with a specific interpreter because they do not find the person to be a good language match or because the Deaf community is small and there may be a potential for dual relationships.
- A client who seems unwilling to work with all available interpreters may be doing so for a variety of reasons—therapeutic resistance may be one of them.
She understands that to work with Mike, she needs more information, so Maria contacts her State Division of the Deaf and Hard of Hearing to consult with their behavioral health and accessibility expert, Vernon. The administrative assistant at the division explains that Vernon will contact her using a video relay service, an accessibility service that provides interpreters to facilitate communication between people who use the phone and people who use video streaming for remote communication. A short time later, an operator/interpreter calls Maria via video relay. The operator explains that Maria is receiving a call from a person who uses sign language to communicate and that she will interpret back and forth between the two of them. The operator is looking at a monitor and can see Vernon, and she is wearing a headset to hear Maria over the phone. The operator explains that Maria should just communicate as though she is talking directly to the caller.
VERNON: [signing] Hi, Maria. I'm Vernon, and I got your message about seeing a Deaf person with a substance use problem. I'll be happy to help with issues of accessibility and any other issues you want to discuss.
MARIA: [through the interpreter] Thanks, Vernon. Yes, I worked with a few Deaf people in graduate school, but there seems to be a lot of new technology, and I'm delighted that you're here to help. For confidentiality purposes, let's refer to my client as “M,” if that's okay with you.
VERNON: Sure.
Master Clinician Note: Maria speaks at a natural pace on the phone. She remembers to clarify with Vernon the meaning of any acronyms she uses, just as she would with anyone who might not be familiar with the lingo or jargon of her field.
MARIA: At the substance use disorder program, we have a standard protocol for assessment, and fortunately, the instruments we use are also available in ASL digitally and are accessible on the Internet. We'll have two interviews to collect data and decide on a treatment plan. We'll need an interpreter for the interviews, and the assessment instruments will be administered during one of the interviews.
How To Identify Your Client's Preferred Methods of Communication When Not In Person
Consider the following issues:
- Can the client talk and hear on the telephone?
- Does the client have access to high-speed Internet, Web cams, and monitors for videophone-based communications? Videophone technology enables ASL users to communicate with each other directly in real time. It is secure and private.
- Does the client typically use a video relay service? Such services combine the use of telephone and videophone technology to facilitate calls between people who communicate in ASL and people who communicate through speech and hearing. Callers dial dedicated numbers that connect them to a relay interpreter who is fluent in spoken English and ASL. The interpreter places and then translates the call. The interpreter sits in front of a Web cam and monitor and wears a headset, enabling him or her to see and be seen by the ASL user and to hear and be heard by the spoken-English user. The technology is secure and private, and the interpreters are certified and adhere to strict ethical guidelines.
- Is the client comfortable communicating in written English? Text messaging or email communication is preferred more commonly by clients who have competence with written English.
- Have you alerted the office staff members at your agency that they may receive calls from video relay services? Some agencies require all clients to work through the front desk to contact their counselors.
- Does your agency allow for appointment communications to happen via email or text messaging? For some Deaf clients, this is more effective and direct than video relay.
VERNON: I'm sending you two email attachments with information about determining your client's preferred way of communicating between sessions and about issues to consider when working with interpreters. You may already know that many Deaf people do not speak English as a primary language and may not understand written notes, including email and text messages.
MARIA: Yes, I remember that from my graduate school days. Okay, I've received your email attachments and I'm looking them over now.
VERNON: Do you know M's comfort level or competence with written English?
MARIA: I know that he graduated from the state school for the Deaf, but I was told by the probation officer that he had a hard time completing the written forms required by the court.
Master Clinician Note: Maria thinks she will need an interpreter for her client to participate in certain aspects of the intake and treatment process. She is aware that the interpreter will not take the place of clinical staff, nor will the interpreter take on roles typically executed by program staff. She also knows that if assessments and materials used in intake, treatment, or continuing care require reading or writing, they may not be appropriate for use with her Deaf client.
VERNON: Be aware that the interview will probably take longer than it would with a hearing client. The interpreter should be there a little early to meet you and work out details. Now, let's move on to the second attachment about issues to consider in working with Deaf clients and interpreters. It's important that you talk with the interpreter about any terminology or acronyms that are specific to what you'll be discussing. Some examples include terms like AA, tolerance, withdrawal, and so on. Many interpreters specialize in mental health and/or addictions work and may have greater facility with the lingo than those who don't have this specific training or skill.
Certified Deaf Interpreters
The Registry of Interpreters for the Deaf certifies trained individuals who are Deaf or hard of hearing to serve as interpreters. CDIs have proficient communication skills, have received interpreter training, and possess knowledge and understanding of Deaf culture and the Deaf community, as well as language fluency to help enhance communication. State departments that oversee services for Deaf individuals can be excellent resources for treatment programs that need interpreter services. For more information, see the Registry of Interpreters for the Deaf Web site (http://www.rid.org/rid-certification-overview/cdi-certification/).
VERNON: Are you familiar with the term “CDI”?
MARIA: No, I'm not.
VERNON: Okay, I think it is important that you know something about Certified Deaf Interpreters. So, I'm sending you another email about working with a CDI.
MARIA: Vernon, I have one last question. If M and I wanted to call the specialized treatment program for Deaf individuals from my office, would it be all right to use Skype? We don't have a videophone here, and I want M to be able to communicate directly with the Deaf and signing staff there if he has any questions.
VERNON: That's a great question. Presently, many individuals who are Deaf and businesses and organizations that employ Deaf people have access to videophones. Unfortunately, Skype does not have the picture or streaming quality of videophones, which can cause choppiness in the sign language. Additionally, Skype doesn't have the security and privacy features that would be necessary for the type of conversation that you and M may need to have with another agency. There are companies that provide secure Web and multiparty video conferencing software and online services. If security isn't a concern, some Deaf clients may choose Skype or iChat to keep in touch with hearing family members. The chat feature enables users to type back and forth in the event that signing is too choppy, or if hearing family members don't sign. This tool can be used when clients are in an inpatient program and want to be able to call hearing family members to talk. It can also be used by Deaf and hearing individuals in recovery for support between meetings.
At the end of their conversation, Maria and Vernon exchange contact information, and Vernon tells her that he will send her links to additional resources. Vernon explains that the best way to reach him is by email for the most immediate response.
Part 2. First session with the client
Maria is ready for her first session with Mike. She has hired an interpreter through her agency. Maria has already chatted with Mike via video relay and has prepared the staff at the front desk to receive both the interpreter and the new client. She has asked the interpreter to come in a few minutes early so that she can review forms and her agenda for the first session. After meeting with Maria, the interpreter returns to the waiting room to wait for the client. When Mike arrives, Maria invites him and the interpreter into the session. She asks Mike and the interpreter what the best seating arrangement would be. Mike requests that the interpreter sit next to Maria across the table, explaining that this will enable him to see both Maria and the interpreter. They begin by completing the intake forms.
How To Set Up the Space To Work With an Interpreter
- Ensure that the room is well-lit with overhead lighting, as opposed to a window as the sole light source—this will prevent anyone from being backlit and in silhouette, which makes it difficult to see faces.
- Leave enough room for each person in the meeting to sit comfortably with the interpreter seated next to the hearing person. The client needs to be able to have visual access to both the counselor and the interpreter.
- Reduce all visual distractions.
- Speak naturally and look directly at the client, directing all communication to the client. Do not ask the interpreter, for example, to “Ask the client if he…” Rather, direct all communication to the client. The interpreter will let you know if your pace is too fast.
- There may be a lag during communication between the interpreter and the client. This may happen for a variety of reasons:
- -
The client may not be familiar with terminology or may use different signs from those the interpreter is using.
- -
The interpreter may need to back up if there was a communication error that needs to be corrected.
- -
The client may be asking questions that are relevant to the communication but not the content.
- It is important to have the Deaf person's attention before speaking. To get a Deaf person's attention, it is appropriate to tap on the shoulder or wave gently. Make sure to look directly at the Deaf person while speaking, even though your natural tendency may be to look at the interpreter. Eye contact is important when communicating with Deaf people. Be aware that if you look away or look elsewhere, it may be distracting for the Deaf person.
MARIA: I'm glad you're here today, Mike. It's nice to meet you.
MIKE: It's nice to meet you, too. I'm not sure how to tell you about my problems. I never had to come to counseling before. I had to come here because everyone says I drink too much, and sometimes I steal pills from my family.
[Mike proceeds to provide Maria with information about his alcohol and drug use.]
MARIA: Lots of people come here because they are having problems related to their alcohol and drug use. We have plenty of time to talk about that, but to begin with, you'll need to complete these forms so that the agency will have all of the information they need about you. These are forms that everyone who comes here completes. Some forms are for insurance, some are for us to know more about you, and some tell you about us and the work we do. Often, people have questions, so I'll be right here in case you need any help.
[Soon after completing basic demographic information, Mike indicates that he doesn't know several of the words or how to spell the answers to the questions. Maria works through the interpreter to help Mike complete the form. She acknowledges that he understands most of the concepts but is not confident in his ability to read and write.]
Substance Use Disorder Screening Tools Developed for Use With Deaf Clients
The Substance Abuse Screener in American Sign Language (SAS-ASL) is an accurate and brief questionnaire specifically developed and validated for the Deaf population to screen for substance use disorders among Deaf adults in behavioral health, vocational rehabilitation, and social service settings. The screener is available through the SASSI Institute Scoring and Report Service (http://www.sassi.com/srs/). Counselors who register to use the Scoring and Report Service can access the link to the SAS-ASL video questionnaire via the Internet and download support materials and the paper version of the questionnaire used by clients to record their responses. Completed questionnaires are sent in for automated scoring, and a report on client results, along with identification of key issues affecting each client, is returned to the counselor via email or fax. It is important to let clients know that this process is secure and confidential.
The Global Appraisal of Individual Needs-Short Screener ASL Version (GAIN-SS-ASL) is a 23-item screening tool to identify mental and substance use disorders. It is administered interactively through Chestnut Health System's Web portal using videotaped clips in ASL; clients answer items by clicking on the choice that best fits them. The instrument screens in four areas: internalizing disorders (e.g., depression, anxiety), externalizing disorders (e.g., attention deficit hyperactivity disorder, conduct disorder), substance use disorders, and crime/violence problems. The instrument is scored via computer, and two narrative reports on the individual's results are produced. Results can be used on the individual level as a measure of change over time and on a quality assurance/program planning level. As a screening instrument, the GAIN-SS-ASL does not provide a diagnosis, but it does accurately identify individuals who most likely have a disorder that would be identified with a longer assessment or clinical interview. Early tests with the GAIN-SS-ASL indicate that the instrument is appropriate for use with adults who are Deaf or hard of hearing and are 18 years of age and older. The written language form of the GAIN-SS-ASL is available in English and Spanish, as well as other languages. For more information on the GAIN-SS-ASL, visit the GAIN Coordinating Center Web site (http://gaincc.org/gainss).
MARIA: Next, we need to find out more about your drug and alcohol use. Today, we are going to use the computer to complete an assessment. You'll watch the monitor and answer the questions, which will be signed in ASL. Then I'll send your answers to a company that scores the assessments. The results will be sent back to me, and we'll look at them before our next session. This will help us to get a better idea about what kinds of treatment options might be best for you. Is this acceptable to you?
MIKE: Wow, that's cool. So I just watch and complete the form? I'm happy that all of this is available for me in ASL. You used video relay to call me, and you have an interpreter, and now this. I really appreciate it all. English is hard for me.
Master Clinician Note: Finding direct, efficient ways to communicate can be frustrating for Deaf clients, who—until recently, with technological advancements—often had to rely on other people and/or antiquated methods to overcome communication challenges. Many (but not all) Deaf people were early adopters of technologies such as computers, handheld devices, and high-speed Internet for video streaming. This has enabled easier communication via email, videophone, and text messaging. Clinicians' willingness to use these technologies enhances access and supports the therapeutic alliance.
MARIA: I'm glad that these things are helping you. It's really important that you be able to fully participate in your treatment.
Before the session ends, Maria tells Mike that they'll discuss the assessment results and plan next steps at their next meeting. She also asks Mike if video relay is a good way for them to communicate. Mike says that video relay is fine and that email and text messages are okay, too. At this time, Maria takes a moment to let Mike know that their communication via email and text will be limited to brief communications about appointment times or quick questions he may have. She explains that email and text messages are not going to be used for counseling because she wants to have direct and comprehensive communication with him whenever possible, and because neither text nor email is confidential.
Part 3. Maria meets with Mike to discuss treatment planning
Maria and Mike discuss his assessment, which indicates that inpatient residential treatment is his best option. Maria presents Mike with two options. The first option allows Mike to go to a community-based inpatient treatment program for hearing people and use a program-provided interpreter for 6 hours a day. This would mean that he could participate in most of the group meetings and some counseling sessions, but there would be no interpreter for events outside the designated 6 hours. He would also be able to attend an interpreted AA meeting if program staff members can drive him there; however, this depends on staffing and available transportation.
Mike wants to know whether there will be other Deaf people in the program and whether friends and family can visit him; he has reservations because, in previous treatment situations, he found it difficult to communicate, and he believed that people were mad at him and thought he didn't try hard enough. He wants to go to treatment closer to home so that it will be easier to get home if he doesn't like it. Maria assures him that treatment is voluntary and that neither program will force him to stay if he doesn't want to.
The second option is for Mike to attend an intensive outpatient program that provides lodging and is designed specifically for Deaf people. Maria knows of a hospital-based treatment program that offers both acute care and residential programs, depending on client need. It is staffed by Deaf and hearing providers who are fluent in sign language so that all group sessions, psychoeducational groups, and individual counseling sessions happen through direct communication. Deaf clients also attend 12-Step meetings in the community, as well as within the general treatment program, which are interpreted by staff interpreters. All staff members, including interpreters, are trained and knowledgeable about Deaf culture, ASL, substance use disorders, and 12-Step culture.
Mike is concerned that leaving the state will be a problem, and he is worried about how he will afford this arrangement. Maria explains that Mike's Medicaid will cover the cost and assures him that she'll work with him to figure out how to cover his airfare expenses.
MIKE: What if these people don't communicate like me? I do all right with my family. We have our own words, but that may not work with people in Minnesota.
MARIA: Mike, I think we'll just have to see how that works. A lot of Deaf people from all over the country go to this program and they seem to do okay. They have videophones and computers and, as I said, all the counselors use ASL.
Substance Use Disorder Resources for Deaf People in Treatment and Recovery
| Organization | Types of Resources |
|---|---|
| MCDPDHHI: http://www | Treatment articles on the Web site, recovery materials in print and via video and live videostreaming on the Web |
| Deaf Off Drugs and Alcohol (DODA): http://www | Deaf AA and support group meetings, daily thoughts/affirmations, and meditation in ASL |
| AA: http://www | Live online chat, interpreted meetings, Web-based Deaf AA meetings |
| E-Michigan Deaf and Hard of Hearing People: http://www | AA steps in ASL videos, 12 Steps interpreted into ASL |
MIKE: Can I come home if I'm not happy there?
MARIA: The program is voluntary, and you can leave if you aren't satisfied with it. In fact, let's call the treatment program now.
Maria and Mike call the intake coordinator at the Deaf-specialized treatment program. Mike participates through the interpreter. The call helps Mike feel comfortable with the decision to go to the specialized program. The intake coordinator also tells Mike about some resources he can use in the days leading up to his departure for Minnesota and emails the list to Maria and Mike.
Part 4. Working with the client to address frustrations
Mike is in Minnesota. Maria has not heard from the treatment program staff, but she has received three emails from Mike, and he has called her twice via video relay. He complains about not feeling as competent as other clients with the language and pace of the program, not feeling included by the group, and not liking that the entire staff knows his business. Mike has told Maria he is going to quit the program. Each time he calls her, Maria asks Mike if he has shared this with his counselor in the program, and he deflects the question. Maria has concerns about diluting Mike's treatment, so she asks if it is okay for the two of them to have a conversation with his counselor. Mike is hesitant, but agrees. Maria reminds him that it is not her practice to have extensive conversations by email or videophone. Mike tells Maria that he will tell his counselor. Mike's counselor is Deaf, so a staff interpreter in Minnesota will translate the call.
Master Clinician Note: Deaf clients in treatment will likely present with the same types and levels of resistance that hearing clients do. It is important that the referring clinician not dilute the treatment process or enable the client not to develop a therapeutic relationship with staff members at the treatment program. Clinicians should remind clients that emails may not be confidential and may not be an effective medium for counseling.
During the phone conversation among Mike, Maria, and Mike's counselor, Mike expresses his fear and resentment, and they agree that Mike needs to bring his concerns to the program staff if he has any hope of getting support. Maria can't help Mike with his problems in treatment, but the program staff can. They agree that Mike and Maria will resume their work together when it is time for discharge. After Mike returns home, he will see Maria for continuing care planning.
The telephone call seems to help Mike feel safer in the program. He understands that the treatment team is working with him and not against him, and he begins to ask for help from the staff and the other clients in the program. He stops complaining, starts to feel connected in a way that he never has before, and begins to value much of what he resisted in the beginning. This feeling of connection extends to his experience at the AA meetings he attends, and soon, he is participating in all aspects of treatment.
Part 5. Helping the client engage with community-based supports
Mike is back home and is at his first meeting with Maria since returning from Minnesota. Maria is working with an interpreter and is discussing the community-based supports that Mike can use in his recovery. She gives him a list of the interpreted AA meetings in the state. The closest interpreted meeting is 20 minutes away, and the other two weekly meetings are almost an hour away. Maria discusses online AA meetings with Mike, and he is ready and able to participate. His plan is to log on to the online AA meetings and the daily Deaf Sober Chat. He has also been enjoying the daily recovery affirmations on the DODA Web site and uses them each day.
MARIA: [speaking to Mike through an interpreter] Well, Mike, you look great. Did you have a good trip home?
MIKE: [signing through an interpreter] Yes. My family was glad to see me.
MARIA: So, you have the list of AA meetings and you are going to attend meetings regularly?
MIKE: I can make the one with an interpreter that's close to my home every week. They only have the interpreter that one time during the week. I'm also going to Deaf AA meetings online.
Maria and Mike discuss the importance of developing a network of people who will help him stay abstinent. Mike explains that the Deaf community is wherever Deaf people are. He is willing to drive some distance to have Deaf sober friends. Mike explains that he learned in treatment that he used alcohol to avoid feelings of isolation and loneliness related to growing up around people without hearing impairment; he had known very few people who could sign, except for when he was at the School for the Deaf. He explains that going to family parties, or even going to community events, left him feeling stupid and alone. He tells Maria that he is not strong enough in his recovery to go to a meeting without other Deaf people, which may make him feel alone again. He doesn't believe he will get any benefit from a meeting that is not accessible. Mike agrees to continue seeing Maria twice a week; as he stabilizes in recovery, the frequency of visits will diminish.
Vignette 5. Using Smartphones To Support Recovery for Clients With CODs
Overview
This vignette illustrates how to use apps to help clients with CODs regulate their emotional responses, to enhance the therapeutic alliance, and to foster clients' use of effective coping strategies. The vignette demonstrates how to help address client resistance to using a mobile phone or tablet app, how the app can be personalized to meet the needs of a specific client, how the app is applied in a crisis situation, and how to motivate counselors to use apps in their practice.
Learning Objectives
- Use apps to assist a client who experiences severe and persistent mental illness.
- Introduce the client to the idea of apps with a mobile phone to support recovery.
- Understand how a mobile phone app can be applied during a client crisis.
- Adapt apps for a wide variety of mental and substance use disorders.
Setting
Betty is a counselor in a comprehensive CMHC that serves several counties. She carries a caseload of approximately 70 clients. Many of these clients are seen weekly, and others, biweekly; she sees a few who are in ongoing recovery on an as-needed basis. Given the size of her caseload, using treatment extenders, or ways to expand treatment beyond weekly or biweekly office visits, is imperative. Treatment extenders are particularly important for clients who need a lot of reassurance, who frequently experience life crises and need immediate support, who need assistance in making everyday decisions, or for whom not being able to access their counselor as needed represents abandonment. Because many people with whom Betty works own mobile phones that can access the Web, she explores Internet apps that can be of use. This vignette demonstrates how she uses some of those apps in her practice.
Joan is a 29-year-old single woman who lives alone and has struggled with depression, bulimia, posttraumatic stress, and alcohol use disorder for the past 8 years. Her alcohol use and other self-destructive behaviors are primarily triggered by posttraumatic stress reactions. After a suicide attempt while intoxicated about a year ago, she began seeing Betty at the CMHC. At first, her attendance was sporadic. Slowly, Joan has become less fearful of treatment, and her relationship with Betty has become very important to her. Although she now attends her treatment appointments regularly, she still has frequent crises in her life, which are often related to interpersonal issues and posttraumatic stress reactions. During these crises, she has few resources to fall back on and is at risk of self-harm through alcohol use, suicidal behavior, and bingeing and purging.
Joan seems to be an ideal candidate for treatment extenders that would help her stay connected to Betty and to her recovery. In the first scene of this vignette, Betty introduces the idea of treatment extenders through mobile phone apps to Joan, and the apps are used during a crisis situation in Joan's life. In the second scene, Joan and Betty discuss, in an office session, how the app worked. Betty then meets with other staff members, describes using treatment extenders, and invites other clinicians to consider how they might use mobile phone or tablet apps.
Betty's Story
Scene 1. Introducing treatment extenders to the client
The session begins with Betty introducing Joan to the idea of incorporating mobile apps into treatment. She explains that they don't replace current treatment, but rather act as adjuncts to support the gains Joan is making and to help Joan manage strong emotions and stress reactions in her life as they occur. Joan has expressed some reluctance about using the apps.
BETTY: So, you seem to have some concerns about this technology that we might use in addition to what we already do. This is not going to take anything away; this is to add on. Tell me a little bit about what your concerns are.
JOAN: My fear is that you're just turning me over to a mechanical device, and I need more than that. I really need your support.
BETTY: So, you're having concerns about being distanced from me or not being able to connect with me if we use this device.
JOAN: Yeah. Because what you're saying is, “Don't call me; press this button instead.”
BETTY: So, if you learn how to use this and get pretty good with it over time, you think there may be more risk of distancing from me. I can understand your fear of losing our connection, but I want to assure you that this isn't going to replace what we currently do in treatment—that is, you seeing me weekly, and the two of us talking on the telephone when you have strong emotional reactions or feel that you are in a crisis. It just supplements that, and perhaps it can help you manage some of those difficult situations better.
JOAN: Well, you've always been honest and straightforward with me. That's been really important to me. It really scares me that I might lose my connection with you.
BETTY: I want you to know that I value our connection. There's no way that I would allow the device to interfere with that. I don't want to be replaced with a machine, either. If we try this mobile apps idea and it isn't working, I'll definitely be the first to say we should drop it. But I really do believe it's going to help, and I want to see you give it a try. I firmly believe that this is a way for you to actually feel more attended to, rather than less.
Master Clinician Note: The counselor walks a fine line between pushing Joan to try the app and allowing Joan's fears to limit her in trying something that could be really helpful. Betty chooses to take a middle-ground approach of encouraging Joan to try the app, but acknowledging that if it isn't working, they can give it up.
JOAN: That sounds good. I'm just still afraid that you're going to be less available to me.
BETTY: The way the app works makes me actually more available, in a sense, because if you're really in trouble, the system can tell me. If you're sensing that you are getting overwhelmed by emotions, you can contact me or the on-call counselor directly. The app will give you, in addition to our relationship, a way to adopt additional coping strategies when you're having trouble. Okay? If you get more distressed—maybe thinking about drinking, binge eating, or feeling overwhelmed with feelings—then access the app and immediately begin the process of getting back into a safer space. The app is just another tool to help you better manage your symptoms.
JOAN: It sounds complicated.
BETTY: Well, let's just take a minute to look at the app.
JOAN: Okay. I just want to be able to talk to you if I'm in crisis or if I feel like I'm losing it.
BETTY: Right. Again, what's the evidence that you have from our prior relationship up to this time that I'm not available to you?
JOAN: Oh, it's not that you haven't been available, although you do remember that you have cancelled appointments on me.
BETTY: Well, sometimes emergencies happen, and there have also been times where I've had to change my schedule around to be able to see you in an emergency. But the bigger issue is that, to the extent I'm able, you can count on me to be there for you, and no app is going to replace that.
JOAN: I do like the idea that maybe I could develop better skills and not be freaking out or getting myself in deeper trouble.
BETTY: So, the idea is to know that the app is there and it's available for you when you need it. At the same time, because you know it's there, you can immediately use the tools to assist in managing difficult situations. So can we agree that we are at a point where you're willing to try the app and see how it works?
JOAN: Yeah, that sounds about right.
BE TTY: I'd like to show you how this tool could work for you. First, let's develop a list of the situations and events that are difficult for you; we can call these trigger events. For each trigger event, let's talk about the coping strategies that tend to work for you—things like coping statements, meditation, and visualization of the ocean, which you've talked about before. We can then enter this information into the app so that you can have reminders for how to cope immediately in those moments when you feel overwhelmed.
[Betty and Joan spend the rest of the session talking about trigger events and identifying effective coping strategies that Joan can use. At the next session, Betty works with Joan to load this information into the app on her mobile phone. They do this on Betty's office desktop computer by simply following the instructions that come with the app. Joan has recorded some self-affirmations and lines of poetry that have helped her manage stressful events in the past. She has also downloaded a photo of her favorite beach. Joan enters all of this information into the app system, which then uploads it onto her mobile phone. Once loaded, Joan sees that the app includes a “My Action Plan” icon. When she clicks on this feature, she sees her trigger situations along with the associated coping tools that she has loaded into the system. Joan is impressed with the other features of the app, including a panic button as well as a “Get Connected” feature that allows her to hear from others who experience similar challenges in coping with strong emotional reactions. She also appreciates that, to increase her phone's security, she has to enter a user name and password that limits others' access to her information.]
Helpful Features in Phone- or Tablet-Based Mobile Applications
- Voice recordings of self-management strategies: people, places, things, mantras, sounds, proverbs, or other self-affirming tools that are personal destressors and support cognitive and emotional regulation and reorganization
- Visuals of soothing people, places, and things to access on demand
- Self-assessments with personalized feedback
- Relaxation exercises and recordings of guided meditations
- Contact list of the user's positive support system
- Interactive goal-setting tool customized to address the user's issues (e.g., identification of triggers, self-identified coping strategies)
- Voice recordings of counselors or others presenting coping reminders
- Peer stories of how others have coped with triggers
- Secured social networks to reduce the user's sense of being alone
- Reminders to the user not to post confidential or sensitive information on unsecure networks
- Secure texting and email functions to facilitate communication with counselors
- Help now/panic button for direct text/call to counselors or other treatment resources
- Camera/video to take pictures of stressful (or peaceful) contexts to send to counselors and/or to compile in a coping skills and resources kit
- Heart rate monitor to help the user regulate breathing
- Virtual (avatar) life coach or chum
- Journal entry function to log events and the user's responses
BETTY: I'd like you to try out this app for a week or so, and when we see each other again, let's talk about what you think of it. I'll be interested in your feedback about using it.
JOAN: I'm willing to give it a whirl.
Master Clinician Note: Technology-based treatment extenders do not replace standard treatment and should augment, but not supercede, the help and support of a counselor. In discussing with clients the use of a treatment extender such as the mobile phone app Betty asks Joan to try, emphasize that you, the counselor, will still be available. However, just as in standard treatment, you may not always be available on a moment's notice. Also be sure to discuss confidentiality and privacy issues related to the use of apps and other technologies, as well as responsibility and accountability for proper use. As with any therapeutic relationship, introduction of a new technology-based strategy needs to be transparent, clearly stated, and offered in the context of a trusting, supportive therapeutic alliance.
Betty and Joan sum up the session and agree on an appointment time for the following week. A couple of weeks later, Joan experiences a crisis. She is blindsided by conflict that she witnesses in a mutual-help program and later identifies the situation as a posttraumatic stress trigger. Rather than leaving the meeting, she decides to try the mobile app and to text Betty. Betty responds with a quick, supportive text message and schedules a brief telephone appointment with Joan for a couple of hours later. She encourages Joan to use the app, particularly with regard to regulating her emotions and getting more grounded. Later that evening, Joan sends a message through the app to Betty saying she is not drinking or engaging in other self-harming behaviors, has used the app, appreciates the brief phone contact with Betty, and has talked with another friend at the meeting, who offered her a different take on the confrontation that occurred at the meeting.
Part 2. A session after the crisis
Joan and Betty are meeting in Betty's office. After some initial settling in, Betty asks about Joan's experience in using the app during the crisis situation earlier that week.
BETTY: So, how's it going? I'm really interested to hear how this phone-based tool worked for you when you had that problem at the meeting earlier in the week.
JOAN: Well, Tuesday, when I almost lost it at the meeting, it was really nice to know that I had some connection to you through this app. When I get triggered, and especially when I'm totally not prepared for it, I really lose it. It's been a problem for me forever, as you know, in relationships. Using the app to help me get grounded really helped. I don't know how much of it was the content on the app and how much of it was just that I had an alternative to feeling out of control, but I really appreciated hearing right then, in the moment, that you would get back to me—and I also appreciated that you then really did get back to me within an hour or two.
BETTY: Right.
JOAN: So, I didn't spiral. That felt really good.
BETTY: How did it feel for you to manage? You went outside just briefly, got yourself re-grounded, went back in, and stayed for the rest of the meeting, which is really something, especially given what you've been through in the past year. How'd it feel to master that?
JOAN: Wonderful. You know my history—I get so reactive in relationships and friendships.
BETTY: Yep.
JOAN: The idea that the app could be there to back me up was really great… the conflict just brought back all this childhood stuff about, “I can't handle this, nobody knows I exist, and I'm going to fall apart, and there's nothing I can do to help that,” and I'm not in that place anymore.
BETTY: So, you felt safer and more able to manage your reactions.
JOAN: Well, the phone felt something like a lifeline. I know it's just a phone, and the app is just an app. But you're right, it is about safety and security for me—and with this, I have something to support me, to fall back on. One thing that really helped is the app's action plan and instructions about what to do and how to handle myself. I liked the idea that we could fine tune the app especially for me, and that we can continue to do so over time as my needs change.
BETTY: I would like for us to focus for a minute on how the app helped you change your thoughts when you saw the conflict. Did you feel the need to run away or feel unable to protect yourself while you were in that situation? What I'm interested in you exploring is how those responses come up and cause thoughts and feelings of being unsafe. When you understand how those thoughts and feelings get triggered, you can then use the app to help you get grounded and refute negative thoughts and feelings.
Using an Action Plan Tool
An action plan tool allows a client (in this case, Joan), in concert with a counselor, to identify and add triggers related to a variety of circumstances, as well as coping strategies for each trigger, into an app. If Joan finds herself in the midst of an emotional, interpersonal, or physical trigger, she can access the tool to remind herself of the coping strategies she and her counselor identified together. The action plan tool thus allows clients to track their own responsivity via the tool, and data about responsivity can be used by counselors as well.
For example, Joan has identified phone calls with her mother, work overload, and lack of sleep as triggers for feeling overwhelmed. She has indicated that breathing exercises and access to her recorded self-affirmations help her settle down after a phone call with her mother. When Joan receives a call from her mother and begins to have the familiar feeling of her stomach tightening, Joan accesses the action plan tool on her phone. She goes through the brief breathing exercise and then listens to the affirmations she has recorded for this trigger. Afterward, she accesses the action plan tracker and records the trigger event, what she was thinking during the event, how she was feeling during the event, and what she did to cope. She then indicates how helpful her response was in calming her down on a scale of 1 to 10. These data are all tracked and logged for future reference.
In a discussion with her counselor, Joan acknowledges that seeing conflicts can also be a trigger for her to feel inadequate and shamed. She adds this trigger to the action plan tool and downloads an audio file featuring sounds of the ocean from the Web to include in her coping toolkit.
Texting and Confidentiality
Texting via cell phones and other devices is quick and convenient—but not secure. Some apps allow for more secure texting and instant messaging, such as demonstrated in this vignette, where text messages are encrypted before sending. However, encryption is not typical in standard mobile phone texting. It is best that, if texting is used at all for counselor-client communication, both parties agree beforehand to a code strategy so that texts divulge minimal information.
Advise clients that text messaging on mobile phones is not encrypted and can be intercepted by others using relatively inexpensive equipment. Text messages can be retrieved by anyone with access to either party's cell phone. Even if the message has been erased, it may still reside in the phone's memory card for a period of time.
[Joan and Betty discuss how, when an emotional or interpersonal interaction triggers a recollection of experiences in her past, Joan begins having feelings about being abandoned, alone, invisible, and unprotected. Behaviors resulting from these emotions lead to trouble, such as attacking others, running away, and self-harming.]
JOAN: I just like the idea that I can handle these situations better. They take such a toll on me, especially in relationships. It's really exciting to know I have options and that I can manage things myself, by using our relationship and the app on my phone.
BETTY: Fantastic. I'm really glad to hear it. It sounds like you're starting to see how this technology can help you. It doesn't interfere with or take away from our relationship, but it can support what we do and put you in charge when it comes to working through tough situations.
Master Clinician Note: To help personalize Joan's action plan tool, her counselor could ask Joan to use the app to document each time she feels overwhelmed with feelings or experiences a posttraumatic stress reaction. She might do this, for instance, for a month. The creation of a marker could then elicit an immediate set of quick self-assessments (e.g., ecological momentary assessments [EMAs]) to gather more details about the event:
- What was the situation that initiated the reaction?
- What thoughts was Joan having?
- What feelings was she having?
- What did she do?
- How did she feel about her response?
EMA data can help Joan and her counselor develop an even more effective action plan for triggers. This type of real-time treatment approach could be very helpful in building an effective collaboration plan.
JOAN: It occurs to me that not having many resources had a lot to do with why I drank all these years. The only way I knew to cope was to drink, but with what I've learned in AA, and what I've gotten from you and the app, I'm learning that I really can control life and my emotions.
BETTY: So you can get through it.
JOAN: Yeah. But still, it's so important for me to know that you were there.
BETTY: Yeah. I'm not planning on going anywhere.
JOAN: You'd better not.
Part 3. Helping clinicians buy in to the use of mobile phone/tablet apps
Betty and four peers meet for group peer supervision. Betty describes how successful the smartphone app has been in helping Joan. Liz, who has also used the app with several clients, offers support.
BETTY: I went to a workshop on helping clients with co-occurring posttraumatic stress and substance use disorders engage more readily in the use of coping skills. In stressful situations, particularly if they also have a history of psychological trauma, they can easily spiral into self-defeating and negative behaviors that alienate them from others. In the workshop, the leader introduced the idea of using computer-based apps to help clients stay more grounded in situations where they otherwise might feel unsafe. When I got back, I looked for clients in my caseload who meet this profile and who might be willing to try an app I found through the workshop.
How To Build Client Buy-In to Adopting Technology in Treatment
- Closely monitor the therapeutic alliance, as you would with any change that might potentially affect the treatment relationship.
- Address what the technology can and cannot do by using clear communication and ensuring transparency. Discuss the client's expectations of how the technology will augment treatment.
- Ensure that the technological application meets client needs.
- Ask for the client's suggestions about how the technology-based tool can be used, eliciting feedback about the tool before actually integrating it into treatment. How can the app be helpful or not so helpful?
- Do some test runs with the tool so that the client knows its purpose and how to use it before incorporating the app into daily use.
- Pay attention to client feedback about interest in using the tool, understanding of instructions about how to use it, perceptions of its use, and expectations about the results of using the app.
- Ensure that the technology is accessible to the client. For instance, does the client have a mobile phone? How does the client normally use the phone, and what would be helpful in terms of its use? What kinds of training might the client need to use the app effectively? Are the language and functioning of the tool or application appropriate for the client? Does the client understand the costs that may be associated with using the technology?
- Explain how the information and data gathered from the technology-based tool will be used in treatment. Discuss ways that this information can build collaboration and self-management in the treatment environment to help the client achieve greater autonomy.
- Clarify who has access to the technology and the information it may collect about the client. What data can the clinician access? What data can the client access? Who authorizes this access, and what is the process for obtaining permission? How can this information be integrated with other records? Can information be shared with another clinician in the case of transfer of care? How long is this information stored? Is it encrypted in resting state? What information, if any, will be integrated into the client's EHR?
Advice to Clinical Supervisors and Program Administrators: Helping Counselors Buy In to Using Mobile Phone Apps as Treatment Supports
- Help counselors see the value of the app for themselves and for their clients.
- Focus on how the app can enhance or augment counselors' jobs—not replace them!
- Elicit counselor feedback about the application and how it can potentially be used; also request feedback on whether they anticipate that it will be helpful or unhelpful.
- Offer training and technological assistance for use of the app with clients.
- Make shared decisions about adopting technology within your behavioral health agency.
- Clearly define measures of success so counselors can monitor effectiveness.
TED: It's an interesting idea. It seems that the key is your belief in the app's ability to help; that made it a lot easier to get buy-in from the client. I think I would need to know more before I could try to convince someone else to use it.
ERIC: I'm also impressed by how well your client has done using this app, and I'd like other clients to use it as well. I think I'd like to learn more about different apps and how to use them—but I'll need help from you and some coaching on how to actually incorporate them into treatment.
BETTY: Maybe we could set up some training sessions. Along with training, you'll really just need to try it out for yourselves. That's what made me a believer. There are lots of other ways to apply apps in a community behavioral health services program like ours—not just with people on the personality disorder spectrum. Of course, we need evidence that an app is effective. Anyone can put an app up on the Web, but it doesn't mean that its effectiveness has been researched.
Master Clinician Note: Other possible uses of apps in behavioral health include:
- As recovery support tools that link people in recovery to virtual support communities; personalized reminders of people, places, and things to avoid; favorite slogans in mutual-help groups; and a variety of supportive Web sites.
- As tools for monitoring and tracking patterns in specific areas of health (e.g., blood pressure, nutrition, blood sugar levels, alcohol consumption, exercise).
- As tracking tools to set personal goals and monitor progress toward them.
REBECCA: I don't know. Will people actually use it when they're in a crisis? It just sounds a little weird to think of someone saying, “Oh, I'm in a crisis, let me use my smartphone app.”
LIZ: I thought exactly that. But I've been using this system with someone who has an extended history with the agency. From what I've noticed over the past couple of months, the number of emergency calls I get from him has gone down. Now, he's more likely to come in and tell me he had a crisis but resolved it on his own. When he begins to feel strong emotions or is in a crisis, he can use the app. The app sends him supportive prompts and has a panic button that will alert me when he's feeling overwhelmed and let me know that I should reach out to him.
Early on, he did hit the button to connect with me, but it wasn't any different from if he called or paged me and got me or whoever was on call. Over the past several weeks, we've done a debriefing after each of the episodes that he's had, and he's feeling really good about being able to ride out episodes of emotional dysregulation successfully, whereas before, he felt overwhelmed in situations that would typically trigger him. He was able to use the app to navigate his way through the situations on his own, but he knew that I was available through the panic button.
He still becomes overwhelmed with feelings at times and needs support to overcome self-defeating thoughts, but he's been able to stay at work or engaged in a conversation instead of storming out of a situation or getting angry. There's a real difference in his capacity to turn to using the app rather than getting explosive. We may want to consider using this app as a team and making it an integral part of our treatment efforts, not just an isolated experiment.
TED: That sounds great, Liz, but what's it going to cost? Does the client have to pay for the app? Who buys the smartphones for people to use?
LIZ: Well, a lot of people already have smartphones today. The other cost is having a data plan that allows people to access the Internet. So, for most people, the cost is minimal.
Master Clinician Note: The difference between smartphones and feature phones is not hard and fast, but smartphones tend to have greater screen size and resolution, higher processing power, and a more powerful and versatile operating system. Many apps require a smartphone. However, technology is rapidly developing, and features and options are quickly evolving toward feature phones having the processing power once reserved for cutting-edge smartphones.
REBECCA: That's great, but I'm not so sure that all our clients will grasp the technology.
LIZ: This just requires using a mobile phone. This is really easy.
BETTY: Very easy.
TED: What about me? I'm not very tech savvy.
BETTY: You don't need to know much of anything that you don't already know. Can you operate a mobile phone or a laptop?
TED: Most of the time.
LIZ: This app was designed to be very user friendly. There's a program that you use on your desktop computer to help the client customize the app so that it helps them respond to triggers with positive coping skills. The beauty of this is that the clients, with a little help from you, come up with their own trigger events, and they devise their own repertoire of coping responses. It's really personalized, not a one-size-fits-all approach. You can update applications on your desktop, or in some cases, the client's computer or even their mobile phone—any system that can access the app. The portability of mobile phones and tablets means that clients could carry coping tools with them wherever they go, even outside the treatment setting, and access them anytime, anywhere. Mobile technology like this could really enhance and extend the work we do.
REBECCA: You actually made a very good pitch.
BETTY: Are there concerns? Does anybody else have issues?
REBECCA: How do I know that it's actually working?
LIZ: Well, it's really up to the client whether to use the device. That's where it becomes really important for clients to buy in to the idea of using the app.
REBECCA: Would I have to remind clients to use it or anything?
BETTY: Like any other treatment effort, you work with the client to help them get the most benefit. As people get comfortable with the app, it becomes more and more of a regular process. You might raise the question of how your client is using the app periodically when you have sessions, but my experience has been that clients want to tell me how it has worked for them.
TED: How do you download the app? Do you plug the client's phone into your computer?
BETTY: Yeah, or you can download it wirelessly by searching for the app through the client's wireless provider storefront. We can even set it—with the client's permission and informed consent, of course—so that you get a flag on your computer when the client is using it. It's client driven; it's there for clients to use when they need it. The client identifies the triggers and the coping skills that will help. The app lets clients build a list of resources, affirmations, supports, and alternatives that are uniquely theirs and are constantly at their disposal. So, every time a client successfully uses the app, they're affirming their own sense of agency and accomplishment.
TED: Are data transmitted back to us? How do we use this? How do you use it in treatment?
Master Clinician Note: Advise clients using apps that may contain confidential information to use a lock and password system on their mobile phone or tablet. Otherwise, anyone with access to the device can use the app and read the content.
BETTY: If your client agrees, you can be notified every time they open the app. Of course, we don't know how well it works until we see the client and ask. But we do know that it's being used. So, when the client comes in, you can say something to the effect of, “Well, I see you opened the app twice last week,” and then you talk about what happened. Perhaps you'll have the opportunity to further customize the app so that it's even more responsive next time.
Examples of Ready-To-Use Behavioral Health Apps
- DBT Diary Card and Skills Coach: Available online (http://itunes.apple.com/us/app/dbt-diary-card-skills-coach/id479013889?mt=8), this customizable dialectical behavioral therapy (DBT) orientation app offers a skills reference guide, an emotions reference guide with tracking capability, and a behavior reference guide with tracking capability.
- DBT Diary: Available from PsychDataSystems, LLC, this app records urges, emotions, and skills used. Clients can review their diary entries at any time and email diary reports to counselors.
- DBT Coach: Available online (http://www.diarycard.net/), this interactive mobile phone app for individuals with borderline personality disorder and a substance use disorder is designed to support and enhance DBT skills.
- PTSD Coach: Available online (http://t2health.dcoe.mil/apps/ptsd-coach), this app was collaboratively developed by T2 and the VA National Center for PTSD to emphasize self-assessment, symptom management, and access to support.
- Breathe2Relax: Available online (http://t2health.dcoe.mil/apps/breathe2relax), this portable stress management tool with hands-on diaphragmatic breathing exercises includes graphics, animation, narration, and videos.
- Stress Tracker: Available at no cost through iTunes (follow the link at http://otswithapps.com/2012/06/25/stress-tracker-app-for-ios-free-and-android/), this cognitive-behavioral therapy app uses mindfulness principles and emphasizes stress management.
LIZ: Right. I think the best feedback I've gotten is when my client comes in and says, “Oh, by the way, I used the app twice last week, but I didn't call you because I didn't need to.”
REBECCA: That sounds pretty convincing, but one thing we're not talking about is that it sounds like this program is going to replace what I've spent years learning to do.
LIZ: Not at all. It's an appropriate resource and extension—but it's not treatment. It's an adjunct, a support. This app doesn't replace the treatment you provide, just as the treatment you provide doesn't only include phone-based counseling. This is just another therapeutic tool; it will never replace the type of therapy that a human counselor can provide. I think we're a long way from when treatment will be achieved by plugging into a computer or mobile phone. There is a lot that we, as providers, can offer our clients that a smartphone app just can't. But there is one thing a smartphone app can do that we can't—be with the client 24 hours a day, 7 days a week.
TED: Good point.
REBECCA: It sounds like it may help in a lot of situations. I'm willing to give it a try.
LIZ: Yeah, this is a chance to try it out. Let's reconvene after a month of each using it on a trial basis with a few clients, and we'll talk again about what we think and how to proceed.
Master Clinician Note: In general, the discussions in this vignette relate to the positive aspects of using mobile apps. However, the possible cons, or pitfalls, for each client or situation need to be taken into consideration. For example, in this particular vignette, Joan is willing to go along with her counselor's obvious interest in giving the app a try, but because Joan may be more sensitive to stress, it is not difficult to imagine some aggravating technological difficulty (e.g., running out of battery power), combined with sudden real-life stressors, increasing rather than decreasing the stress of a difficult situation for Joan. In-session rehearsals focused on how to manage or respond to the likely occurrence of app or other technological problems are warranted. Remember that what may be beneficial for one client may not be for another. For example, the use of an app could worsen a client's tendency to isolate or avoid social interactions. You must always assess the appropriateness of using any app in the context of the client's perspectives and possible reactions. (See also Part 2, Chapter 2, “Determining the Appropriateness of TAC for Clients.”)
- Introduction
- Implementing a Web-Based Prevention, Outreach, and Early Intervention Program for Young Adults
- Using Computerized Check-In and Monitoring in an Extended Recovery Program
- Conducting a Telephone- and Videoconference-Based Pretreatment Group for Clients With Substance Use Disorders
- Incorporating TAC Into Behavioral Health Services for Clients Who Are Hearing Impaired
- Using Smartphones To Support Recovery for Clients With CODs
- Part 1, Chapter 2 - Using Technology-Based Therapeutic Tools in Behavioral Healt...Part 1, Chapter 2 - Using Technology-Based Therapeutic Tools in Behavioral Health Services
Your browsing activity is empty.
Activity recording is turned off.
See more...