From: Induced innate responses to infection

NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
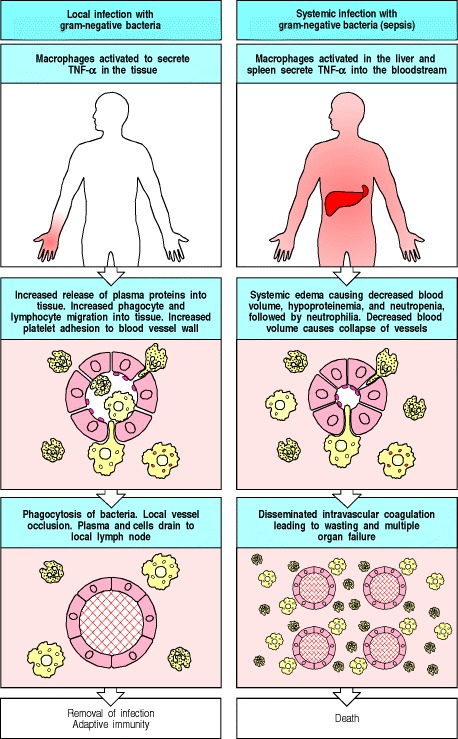
The panels on the left show the causes and consequences of local release of TNF-α, while the panels on the right show the causes and consequences of systemic release. Both left and right central panels illustrate the common effects of TNF-α, which acts on blood vessels, especially venules, to increase blood flow, to increase vascular permeability to fluid, proteins, and cells, and to increase endothelial adhesiveness for leukocytes and platelets. Local release thus allows an influx into the infected tissue of fluid, cells, and proteins that participate in host defense. Later, blood clots form in the small vessels, preventing spread of the infection via the blood, and the accumulated fluid and cells drain to regional lymph nodes where the adaptive immune response is initiated. When there is a systemic infection, or sepsis, with bacteria that elicit TNF-α production, then TNF-α is released into the blood by macrophages in the liver and spleen and acts in a similar way on all small blood vessels. The result is shock, disseminated intravascular coagulation with depletion of clotting factors and consequent bleeding, multiple organ failure, and frequently death. These effects require the presence of the TLR-4 protein on macrophages, which provides the initial signal in response to LPS.
From: Induced innate responses to infection

NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.